Heart failure in chronic kidney disease
Heart failure in chronic kidney disease
ക്രോണിക് കിഡ്നി ഡിസീസിൽ ഹാർട്ട് ഫെയ്ലർ
Prevalence of both heart failure and chronic kidney disease (CKD) are increasing as the population is aging globally. Hence heart failure in chronic kidney disease is seen more often. Presence of CKD in heart failure increases illness and mortality. Though there is increasing use of effective medications and special devices like heart failure device in heart failure patients in general, those with CKD have not been benefitted well.
CKD is defined as abnormalities of kidney structure or function, present for >3 months, with implications for health. The markers of kidney damage include passing a protein known as albumin in urine, abnormalities seen on urine microscopy, abnormalities noted in kidney biopsy, and abnormalities of kidney structure noted on ultrasound scanning or other imaging tests.
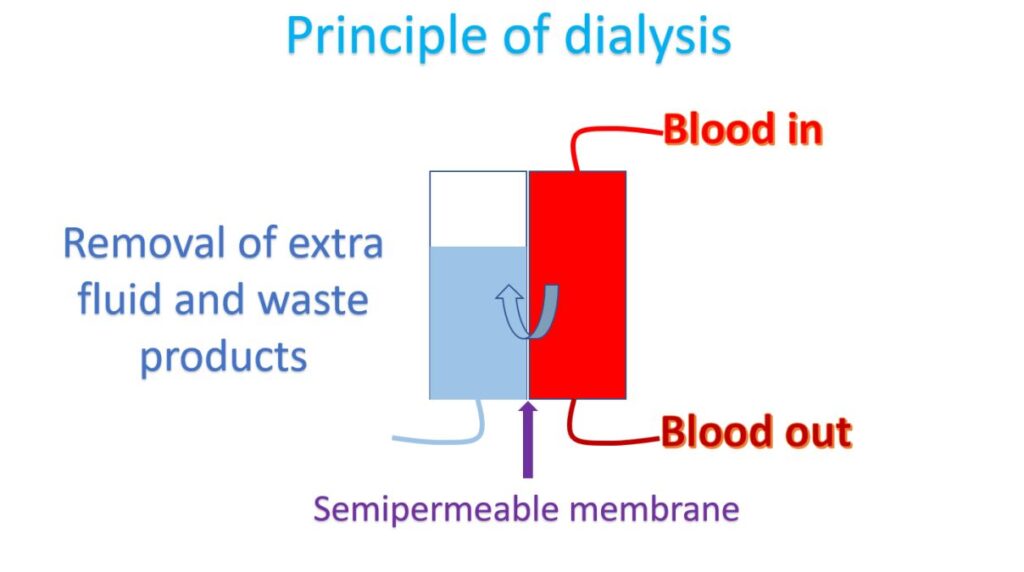
Heart failure can occur in those on dialysis as well as those who have kidney disease not requiring dialysis. Naturally those on dialysis have more advanced kidney disease. Major medications used in heart failure can also be used in those with heart failure and mild-moderate CKD. But caution is needed because some of these medications can cause a rise in blood potassium levels. Some may occasionally lead to transient worsening of kidney function as well.
Another group of medications needed when there is a combination of heart failure and kidney disease are those which increase urine output, known as diuretics. Often a combination of these medications and higher doses are needed in CKD with heart failure, to get relief from the extra fluid retention. In that situation close monitoring for worsening kidney function and abnormality in blood electrolytes (sodium, potassium etc.) is needed.
Those with CKD often have associated anemia (low hemoglobin) as kidney is involved in synthesis of a hormone which promotes the production of red blood cells in the body. Giving iron containing medications as a drip through the veins intermittently have been found to reduce the need for hospital admissions due to heart failure in CKD significantly. Treatment with iron containing medications is also useful in improving symptoms of heart failure with CKD.
Heart failure device is otherwise known as cardiac resynchronization therapy as it synchronized the contractions of different parts of the left ventricle by giving appropriately timed electrical signals. Left ventricle is the lower left heart chamber which pumps blood to the whole body. The procedure is done by implanting a device under the skin and connecting with three lead wires introduced through veins into three chambers of the heart. The expensive device can be implanted only in eligible patients with heart failure as determined by tests like ECG (electrical recording of the heart) and echocardiogram (ultrasound scan of heart). The device has been shown to reduce mortality and hospitalizations in heart failure patients with CKD.
Another method which can used to remove excess fluid from the body in patients with CKD is peritoneal dialysis. In peritoneal dialysis, a special fluid is put inside the tummy using an implanted tube. Peritoneum is the inner lining of the tummy outside the intestines. Peritoneum can exchange extra fluid into the special fluid. The fluid is drained after a few hours, removing waste products and excess water. This can be done at home by the care taker if the tube has been placed from the hospital. But care has to be taken to avoid removing too much fluid as it can lead to fall in the blood pressure. Advice from the treating doctor has to be followed in this regard.
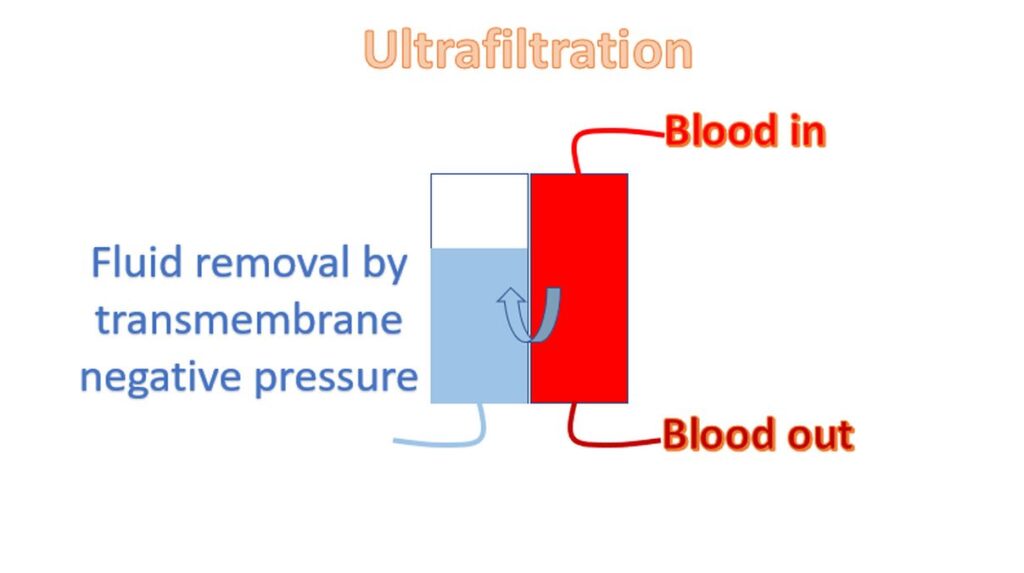
Another special technique to remove excess fluid from the body in CKD patients with heart failure is by ultrafiltration during usual dialysis from the hospital or dialysis centre. This is done by giving negative pressure across the dialysis membrane by the dialysis machine. Same caution is needed in this case also to avoid removing too much fluid, which can lead to fall in blood pressure.