Mitral Stenosis
Mitral Stenosis
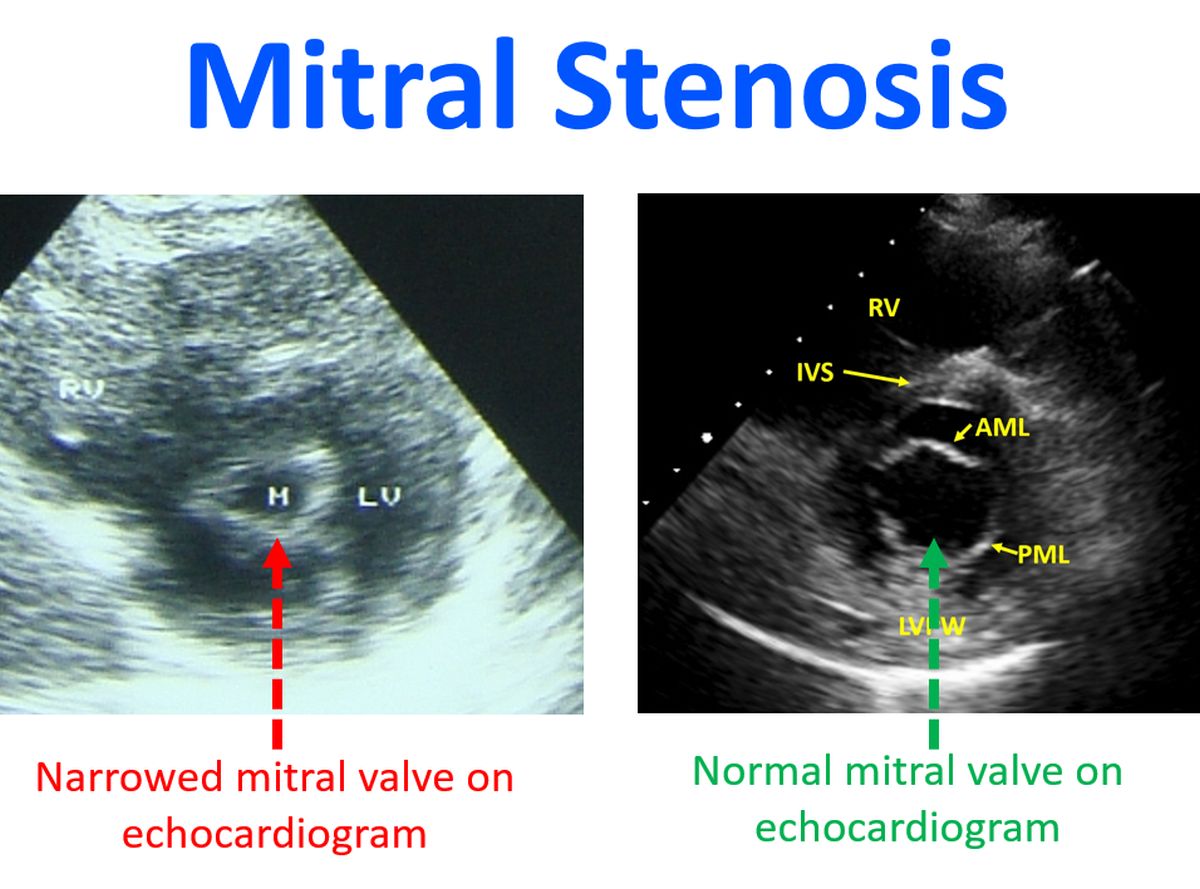
Mitral stenosis is narrowing of the mitral valve between left upper and lower chambers of the heart. The commonest cause of mitral stenosis is rheumatic fever. Congenital MS occurs in a very small group and other causes are extremely rare. Hence if MS is documented, especially in the developing countries, it is most often of rheumatic etiology. Mitral stenosis can be documented well by echocardiogram, ultrasound imaging of the heart, as seen in the picture.
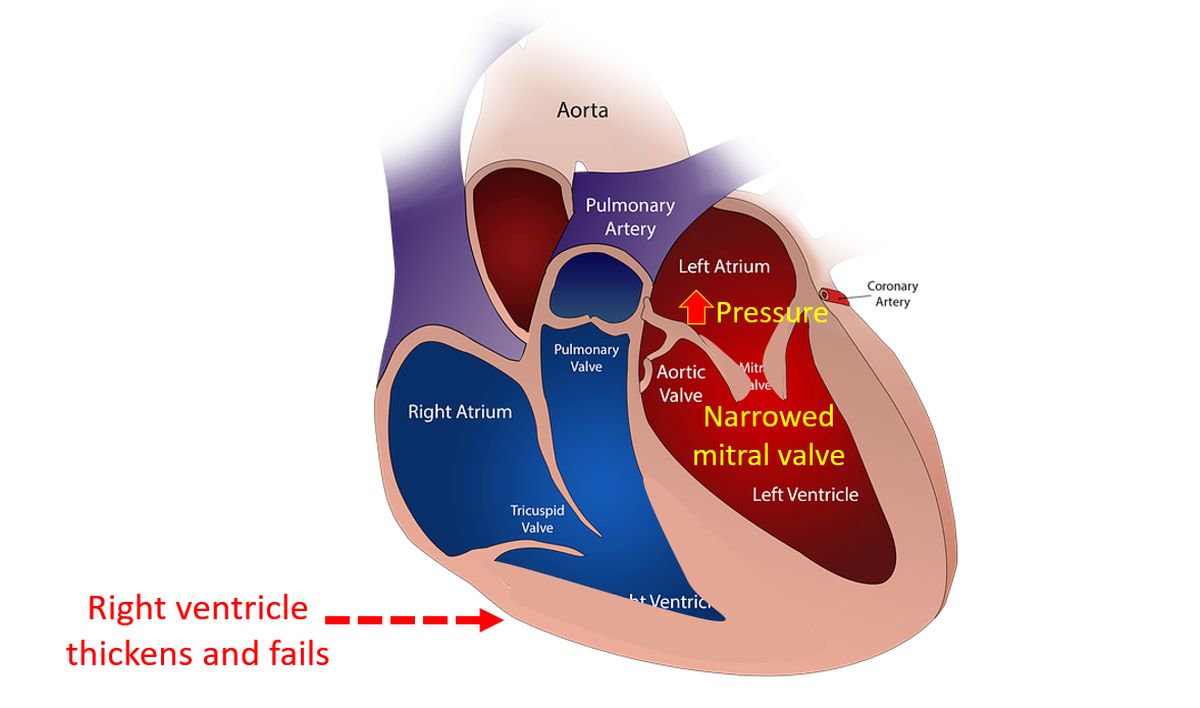
As the mitral valve becomes narrow, the pressure in the left atrium and consequently that in the pulmonary veins and capillaries rise. When the pulmonary capillary pressure reaches above 25 mm Hg, there is a chance for transudation of fluid into pulmonary alveoli. This is known as pulmonary edema and causes severe breathlessness. To begin with this occurs only during exercise while later on when the severity of mitral stenosis increases, this can occur at rest as well. Usually this occurs when the mitral valve area has gone below 1 sq cm. Hence a valve area less than 1 sq cm constitutes critical mitral stenosis. When the pulmonary capillary pressure is chronically elevated, it leads to reactive pulmonary arterial hypertension and right ventricular failure as a consequence.
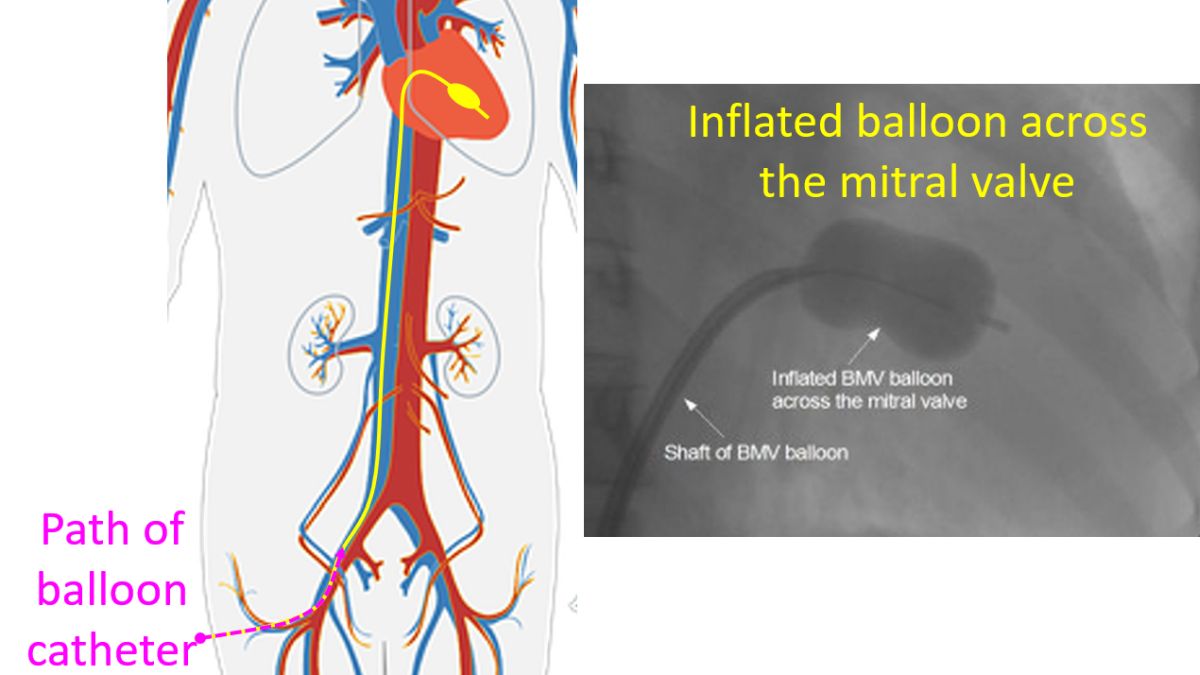
The modern treatment of mitral stenosis is balloon mitral valvotomy if the valve is pliable and non-calcified. It is a non-surgical treatment done from the cardiac catheterization laboratory. The valve is enlarged by a balloon indroduced under X-ray guidance through a nick in the groin. The balloon catheter moves through the femoral vein in the groin, through the inferior vena cava, into the right atrium. Then it reaches the left atrium and left ventricle through a puncture made in the inter atrial septum. When the deflated balloon is across the mitral valve, it is inflated and then quickly deflated, relieving the obtstruction to mitral valve.
If the valve is calcified, attempts of balloon valvotomy may sometimes result in severe mitral regurgitation due to leaflet tear. This mandates urgent valve replacement. Hence elective mitral valve replacement is often resorted to in calcific mitral stenosis. If the mitral valve is replaced by a mechanical prosthetic valve, lifelong anticoagulation with regular monitoring of clotting function with prothrombin time estimation is needed.



