What is an implantable cardioverter defibrillator (ICD)?
What is an implantable cardioverter defibrillator (ICD)?
എന്താണ് ഇംപ്ലാന്റ് ചെയ്യാവുന്ന കാർഡിയോവർട്ടർ ഡിഫിബ്രിലേറ്റർ (ICD)?
इम्प्लांटेबल कार्डियोवर्टर डिफिब्रिलेटर (ICD) क्या है?
Implantable cardioverter defibrillator (ICD) is a cardiac implantable electronic device (CIED). The device is implanted in under the skin under local anaesthesia, below the left collar bone. The electrode lead from the device is introduced into the right sided chambers of the heart through a vein behind the left collar bone. Vein is a blood vessel carrying deoxygenated blood to the heart. The device senses the heart rhythm automatically. It can detect life threatening abnormalities in the heart rhythm and treat them electrically. If a certain abnormal rhythm from the lower chambers of the heart known as ventricular tachycardia is detected, the ICD tries to overdrive it by fast pacing. Pacing is giving regular electrical pulses to the heart through the leads. If it does not suppress the ventricular tachycardia, the ICD delivers a shock through its high voltage coil within the heart.
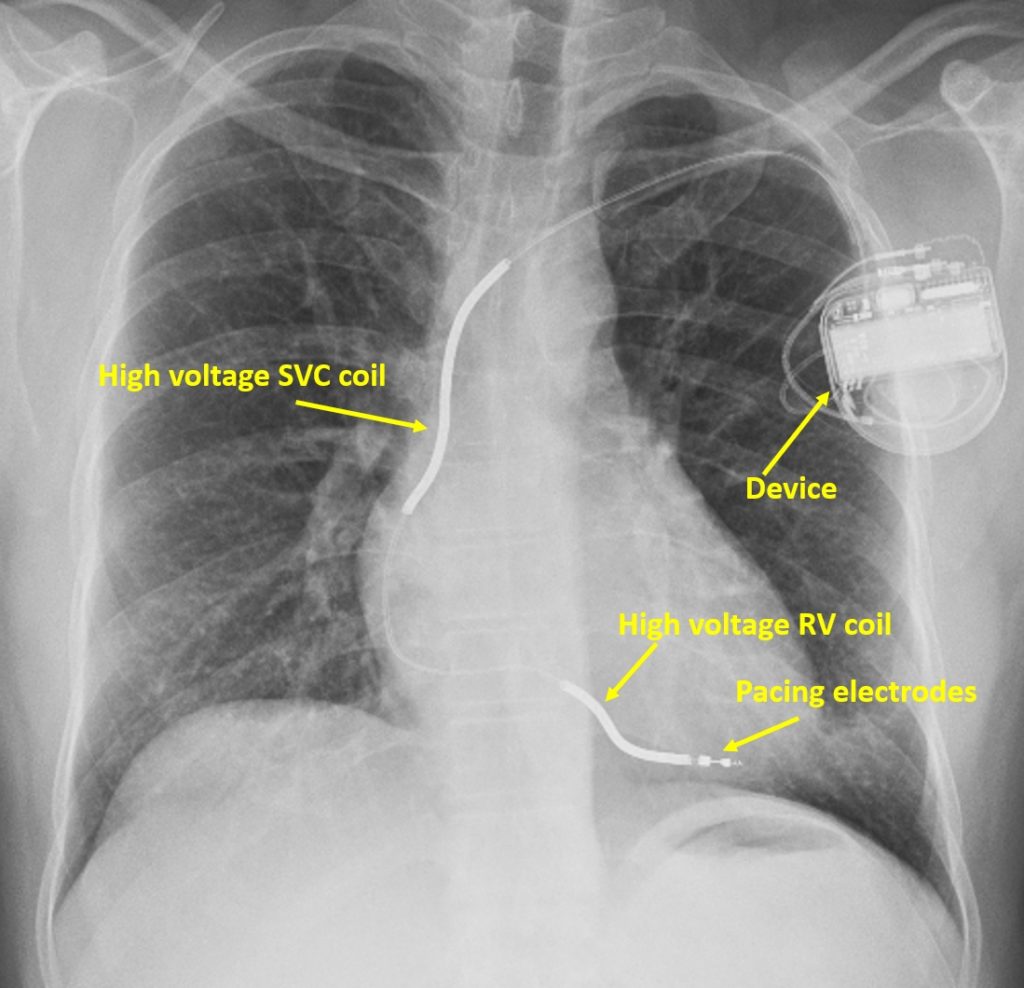
The X-ray picture shown above depicts a high voltage coil in the superior vena cava. Superior vena cava is the blood vessel carrying deoxygenated blood from upper part of the body to the heart. There is another coil in the right ventricle, the right lower chamber of the heart. ICDs can also give back up pacing if the heart rate is very low for a short period of time after a shock. Pacing electrodes are seen at the tip of the lead in the X-ray.
If a life threatening rhythm from the lower chambers of the heart known as ventricular fibrillation is detected by the ICD, it immediately gives a shock to correct the rhythm. Thus the ICD is an important life saving device which safeguards the recipient from sudden death by dangerous abnormal electrical rhythms of the heart. Occasionally, an ICD may give an inappropriate shock when actually one is not needed. These can be averted to some extent by meticulous device programming. Some do have psychological problems due to the fear of shocks. Good counselling is often useful to allay this anxiety.
The most commonly implanted ICD is also called transvenous ICD because the leads are introduced through the veins into the heart. A purely subcutaneous ICD with lead implanted under the skin on the left side of the chest is also available. Recently an extravascular ICD has been tested, with a lead underneath the breast bone, with performance better than purely subcutaneous ICD and almost nearing the transvenous ICD.
These new types of ICDs have been innovated to avoid the potential problems with leads within the blood vessels and heart in conventional ICD system. Leads inside the blood vessels can get infected, can get fractured or dislodged and occasionally perforate the heart chambers. Leads can also lead to formation of clots within the heart and blood vessels. For these reasons, lead has been called as the ‘Achilles Heel’ of most cardiac implantable electronic devices or CIEDs, which include pacemakers and ICDs.
The ICD system consists of a pulse generator with battery, usually implanted below the left collar bone for transvenous ICDs. Pulse generator is implanted below the left armpit in case of purely subcutaneous ICD and extravascular ICD. Left sided implants are preferred because ICD shocks will be more effective with an ICD pulse generator can on the left side. ICD pulse generator can is one active electrode while high voltage coils located in superior vena cava and right ventricle are the other active shock electrodes for a transvenous ICD.
Overdrive pacing for ventricular tachycardia is an option available in transvenous and extravascular ICDs, but not in purely subcutaneous ICDs. Overdrive pacing is a painless form of treatment for ventricular tachycardia which is not too fast. Most ICDs can be programmed to try overdrive pacing when the high voltage capacitor is being charged for shock delivery. If overdrive pacing is able to terminate the ventricular tachycardia, a shock is averted. All fast ventricular tachycardias and ventricular fibrillation usually receive shock as the first option.
The battery life of the ICD depends on the number shocks it is called upon to deliver and the energy levels needed for each shock. Medications can be used to suppress ventricular tachycardia to reduce the potential need for shocks. But there is a caveat. Breakthrough ventricular tachycardia can occur at a lower rate, below the programmed detection rate of the ICD. Recurrent slow ventricular tachycardia potentially reduces the pumping function of the heart and cause heart failure in the long run. Medications can also sometimes increase the energy needed for the shocks to terminate a life threatening heart rhythm.
Another option often used to reduce the number of ICD shocks is mapping the site of origin of the ventricular tachycardia using electrodes introduced into the heart known as electrophysiology study. The abnormal focus can then be removed by delivering short pulses of energy using radiofrequency current, known as radiofrequency catheter ablation. This does not have the disadvantages mentioned in case of medications. But mapping and ablation may not be that successful in all cases.
Good follow up programming is a must in case of ICD. ICD programming is done by a device which sent radio signals to the device and receives information stored in it. ICD interrogation is needed after each shock to ascertain whether it was appropriate or inappropriate. Interrogation is also needed to check battery status. Recorded events can give an idea of the types of heart rhythm abnormalities.
With modern ICDs remote follow up is also possible with basic data from the ICD being transmitted over a wireless network to a physician located even in another continent. But changing programmed parameters will need a visit to the nearest specialist centre. Wireless access to medical devices have always raised concerns about unauthorized malicious access.
Another concern about ICDs is during end of life care. There may be situations in which ICDs may have to be inactivated in a near terminal situation, raising ethical concerns. Like a pacemaker, ICD has to be explanted when cremation is being planned. Care has to be taken to suspend ICD shocks by programming to avoid shocks to the persons doing the explantation. In other situations like while surgery using electrical devices used to control bleeding are being planned, it is possible to suspend ICD shocks by applying a magnet over the ICD, when a programmer is not available.
Precautions with electromagnetic radiation and magnetic resonance imaging are applicable to ICDs like pacemakers. This is because electromagnetic waves can interfere with functioning of the ICD. It can also interfere with the communication between the ICD and the programming device. Mobile phones can be used on the opposite ear, at a distance of at least 15 cm from the location of the ICD. Person with ICD should not drive a vehicle if an ICD shock has been received in the preceding few months. Beyond that period, opinion should be sought from the doctor who is following up the device function. This is only a brief overview about ICDs as the topic is very vast!



