What is HOCM?
What is HOCM?
HOCM is short form for hypertrophic obstructive cardiomyopathy. Cardiomyopathy means heart muscle disease. Hypertrophy means increased thickness. So HOCM is a disease in which the left ventricular muscle is thickened and produces obstruction to the outflow of blood to the aorta. Left ventricle is the left lower chamber of the heart which pumps blood to the aorta. Aorta is the large blood vessel arising from the left ventricle which takes blood to the whole body. An important symptom of HOCM is breathlessness on exertion.
HOCM is an inherited disease which can affect 50% of first degree relatives. First degree relatives mean father, mother, brother, sister, son and daughter. A variety of the disease without obstruction to the outflow of blood from the left ventricle is called hypertrophic non-obstructive cardiomyopathy or HNOCM. HOCM is also mentioned as ‘hocum’ Both together are known as hypertrophic cardiomyopathy or HCM. HCM may occur in about one in five hundred persons in general population. Though both forms have significant risk, risk is more for HOCM. HOCM may be associated with leak of the mitral valve. Mitral valve is the valve between the left upper and lower chambers of the heart.
Hypertrophic cardiomyopathy is an important cause for sudden death in young athletes. That is why pre-participation screening for athletes is being considered in several places. This is very important if there is a family history. Hypertrophic cardiomyopathy can cause dizziness during exertion and more so while taking rest after exertion. This can be associated with dangerous heart rhythm abnormalities originating from the lower chambers of the heart. Another heart rhythm abnormality which can occur is from the upper chambers of the heart known as atrial fibrillation. Onset of atrial fibrillation can worsen the physical status very much in HOCM.
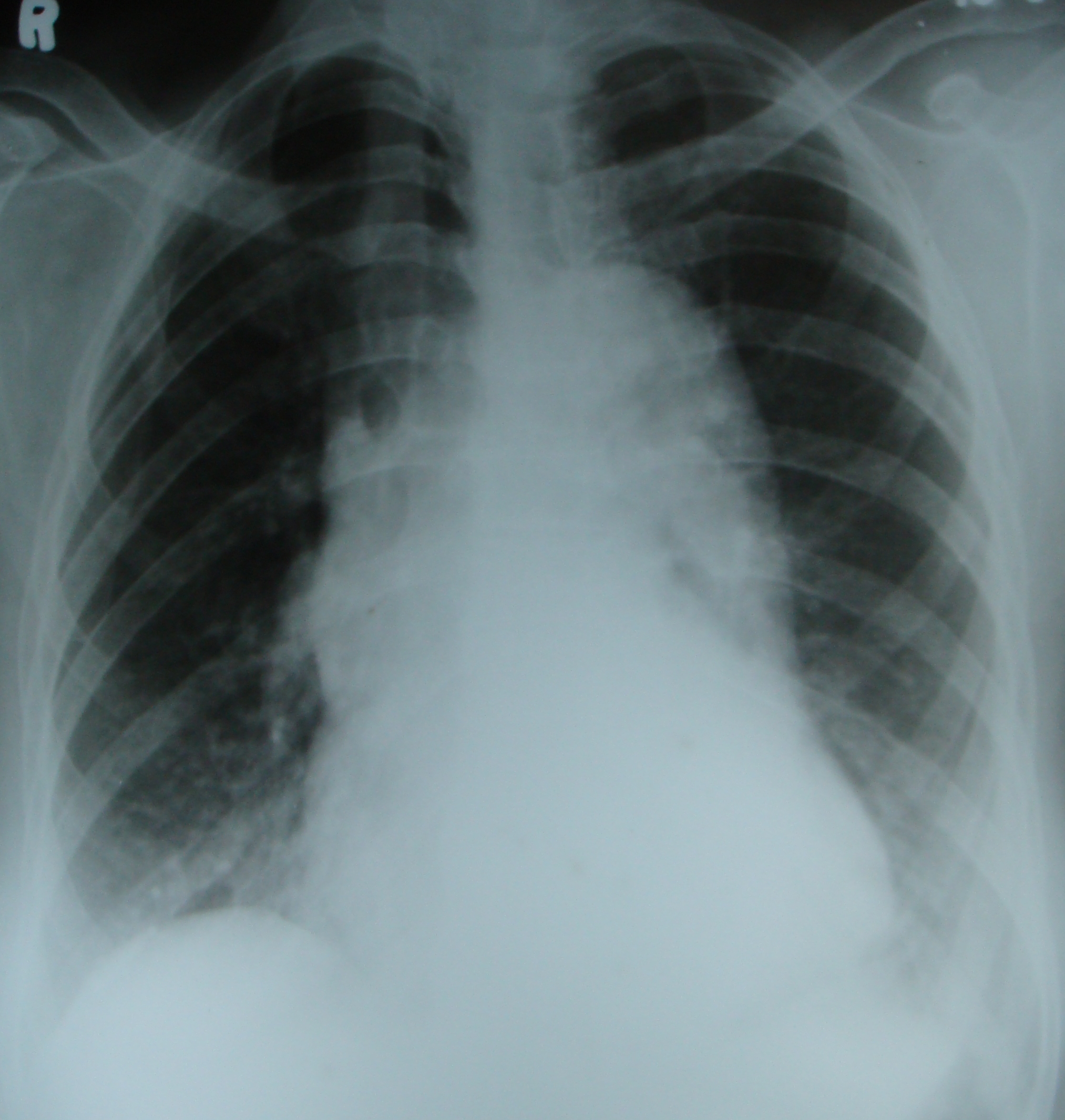
In HOCM, the thickened heart muscle has difficulty in relaxing and receiving blood from upper chambers when it relaxes after a contraction. This causes reduction in filling of the lower chambers and elevation of pressures in the upper chambers. Increase in pressure in left upper chamber or left atrium is transmitted back to the blood vessels of the lungs. Consequent increase in pressure of blood vessels of lungs is a cause for breathlessness on exertion. Upper chambers contract more forcefully to improve filling of the lower chambers.
This is atrial help for ventricular filling, which is lost when there is atrial fibrillation. In atrial fibrillation, the electrical activity of upper chambers is very fast, irregular and disorganized. This causes a standstill of the upper chambers. Thus there is a loss of atrial help to ventricular filling in atrial fibrillation. Loss of atrial help reduces the ventricular filling in the thickened left ventricle in HOCM and may cause a decrease in the amount of blood pumped out. Reduction in the blood pumped out may cause dizziness and fall in blood pressure. That is why atrial fibrillation is so bad in HOCM.
Important symptoms of hypertrophic cardiomyopathy are chest pain, mostly on exertion, shortness of breath, fatigue, giddiness, and abnormal heart rhythms known as arrhythmias, causing palpitation. In the late stages when the heart fails, swelling of the ankles, legs and tummy may occur due to fluid collection. Many persons with hypertrophic cardiomyopathy may be asymptomatic. These persons are identified either during a family screening or on routine medical check-up for other reasons.
HOCM can be suspected during physical examination when a heart murmur is detected. There may be no murmur in the non-obstructive variety. Both will show electrical evidence of left ventricular hypertrophy or increased thickness on ECG. Echocardiogram or ultrasound imaging of the heart will show the increased left ventricular thickness, obstruction to left ventricular outflow and leak in the mitral valve in HOCM. Mitral valve is the valve between the left atrium and left ventricle.
HOCM can be treated by medications which decrease the force of contraction of the left ventricle and thereby decrease the left ventricular outflow obstruction. In atrial fibrillation, if the heart rate is very fast, it can be controlled by medications. Those with atrial fibrillation may be given medications to prevent clot formation in the heart. This is because the upper chambers are at standstill in atrial fibrillation and promotes clot formation. Clots can move out of the heart and block blood vessels elsewhere and produce conditions like stroke.
Advanced form of treatments in the few HOCM patients not responding to medications is a surgery known as septal myectomy and an interventional procedure known as alcohol septal ablation. Septal myectomy is a major open heart surgery requiring great expertise, but having better long term results. Alcohol septal ablation is done using small tubes introduced through blood vessels and injecting tiny amount of absolute alcohol into a small blood vessel of the heart to block it. This causes damage to a portion of the wall between the two lower chambers of the heart known as interventricular septum, reducing the obstruction in HOCM.
Alcohol septal ablation is also an advanced procedure with some risk. If extensive area of damage is caused in the septum or wall between the two lower chambers, it can be harmful. Large area of damage may cause heart failure. Scar formation in the region can occasionally lead on to dangerous heart rhythm abnormalities. Occasionally the damage may extend to the electrical conduction system of the heart to produce complete heart block. In complete heart block, electrical signals from the upper part of the heart will not reach the ventricles and will need the implantation of an artificial permanent pacemaker.
Heart rhythm abnormalities originating from the lower chambers of the heart in HOCM can be dangerous sometimes. In addition to medications, these can be treated by implanting a device known as implantable cardioverter defibrillator or ICD. The device is usually implanted under the skin of the chest and connected to the heart chambers through lead wires introduced through the blood vessels. ICD, also known as AICD as it functions automatically, monitors heart rhythm continuously and treats heart rhythm abnormalities. If a fast rhythm from the ventricles is observed, it will first try to suppress it by giving regular signals at a faster rate, known as overdrive pacing. In case it does not work, an internal electric shock is given to abolish the dangerous heart rhythm.