Supraventricular ectopics
Supraventricular ectopics are the commonest form of supraventricular arrhythmia. They can occur in isolation or in sequences of couplets. If more than three are seen in a sequence it will constitute a short run of supraventricular tachycardia. Supraventricular ectopics are common in the setting of atrial dilatation due to chronic obstructive lung disease or left ventricular dysfunction. Supraventricular ectopic beats have a narrow QRS complex preceded by an abnormal P wave. Sometimes the P wave is not visible if it is not hidden within a QRS complex or T wave. The ectopic beat is followed by a compensatory pause which is classically not fully compensatory, unlike a ventricular ectopic beat.
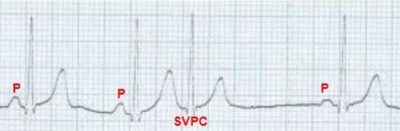
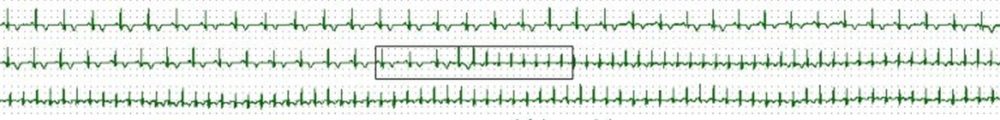
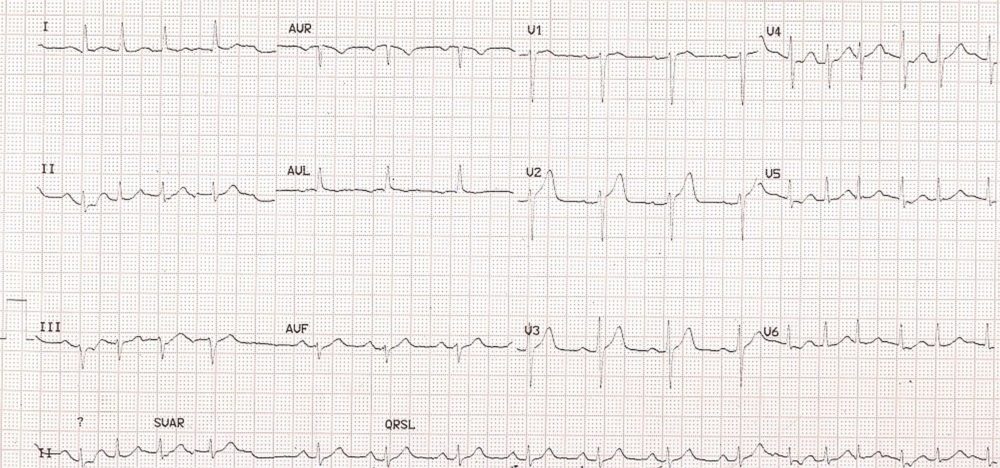
Supraventricular ectopic beat (SVPC) with a narrow QRS complex and no evident P wave preceding it. It is followed by a pause which is not fully compensated.
Supraventricular ectopics: The lead II rhythm strip at the bottom of the images shows two premature complexes (4th and 11th). These premature complexes are narrow and resemble to QRS complexes of the sinus rhythm. Hence they are supraventricular ectopic beats. Ventricular ectopic beats are bizarre and wide, totally different from the QRS complexes in sinus rhythm. Supraventricular ectopic beats originating in the atrium or upper part of the AV junction have P waves preceding the QRS complexes. But these need may be submerged in the T wave of the preceding beat. Mid junctional beats have their P waves within the QRS complex and hence obscure. In a low junctional rhythm inverted P waves can be seen after the QRS with a short PR interval. In the current tracing, no definite P waves belonging to the ectopic beat are discernible. The premature beat is followed by a compensatory pause which is less than fully compensated in that it is about 120 ms less than twice the regular sinus cycle length. In ventricular ectopic beats, the pauses are fully compensatory meaning that the coupling interval between the preceding normal beat and the ectopic beat added to the pause will be exactly twice the regular sinus cycle length. This is because the ventricular ectopic beat seldom gets conducted back to the sinus node to reset it or it reaches there late after the sinus beat has already occurred and captured the atrium. In contrast, the supraventricular ectopic beat usually discharges the sinus node prematurely and resets the sinus cycle so that the pause is less than fully compensated. The difference in the length of the pause from the sinus cycle length depends on the time taken for the supraventricular ectopic beat to travel up to the region of the sinus node, at which point the sinus cycle restarts. The pause can be lengthier if there is suppression of the sinus node activity by the ectopic discharge as in sinus node dysfunction.This ECG also shows deep S waves in V2 and V3 as well as tall T waves in V3 and V4. But the pattern is more of a normal variant than that which could occur in hyperkalemia and hyperacute phase of myocardial infarction. The latter condition is often missed and mandates a repeat ECG if the clinical condition is suggestive.
Supraventricular tachycardia
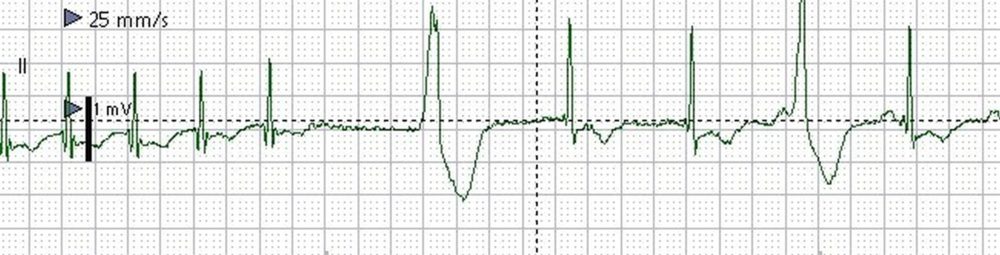
Supraventricular tachycardia (SVT) can be recognized on the ECG by a narrow QRS tachycardia with either absent P waves or P waves which are distinctly different from those in sinus rhythm. Often P waves are not visible in supraventricular tachycardia because the commonest form is atrioventricular reentrant tachycardia (AVNRT) in which P waves are masked by the QRS complex. A close scrutiny of the terminal portion of QRS complex will reveal retrograde P waves which will be inverted in inferior leads and positive in V1. These have been called pseudo s and pseudo r’ waves in supraventricular tachycardia.
ST segment depression is common with supraventricular tachycardia, and it need not indicate associated coronary artery disease. Atrial repolarization wave which is not visible in a usual ECG could become prominent during supraventricular tachycardia and contribute to the ST segment depression which is often associated with it. Post conversion ECG is usually normal unless there is associated ventricular pre-excitation (Wolff-Parkinson-White syndrome or WPW syndrome).
Supraventricular tachycardias have been classified into long RP and short RP tachycardias depending on whether RP interval is longer or shorter than PR interval. Typical form of AVNRT is the commonest form of short RP tachycardia. But P waves are visible only 20% of them.
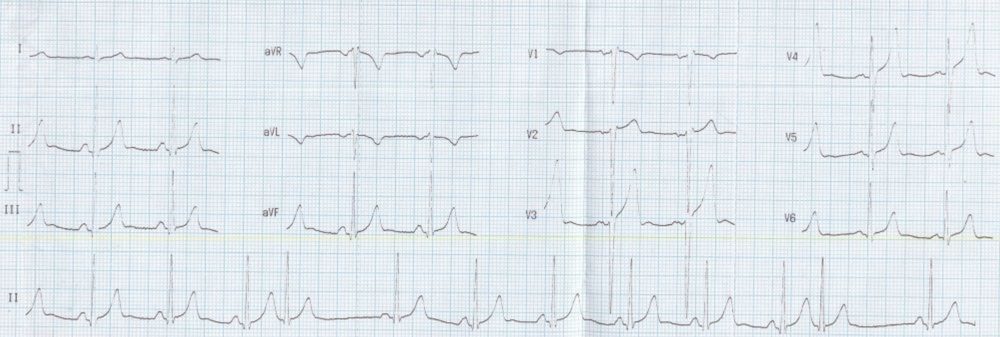
Supraventricular tachycardia with narrow QRS complexes. ST segment depression in inferior and lateral leads, need not indicate ischemia.
Supraventricular tachycardia with aberrant ventricular conduction
ECG diagnosis of supraventricular tachycardia becomes difficult when it is associated with aberrant ventricular conduction as it appears as a wide QRS tachycardia. It may be noted that wide QRS tachycardia is usually taken as ventricular tachycardia unless proved otherwise. If typical right bundle branch block pattern is seen as in the illustration, it is easy to make a diagnosis of supraventricular tachycardia with aberrancy. Otherwise it is often difficult to make a diagnosis of supraventricular tachycardia with aberrancy, especially in an emergency situation. When in doubt, it is better to treat by direct current cardioversion if there is hemodynamic compromise. Diligent search for dissociated P waves, if found, could favour a diagnosis of ventricular tachycardia. But this is often difficult in a fast rhythm, which could be further confounded by frequent artefacts in a restless person. Diagnostic use of adenosine has been recommended, but is not totally without risk as rarely, adenosine associated ventricular fibrillation can occur.
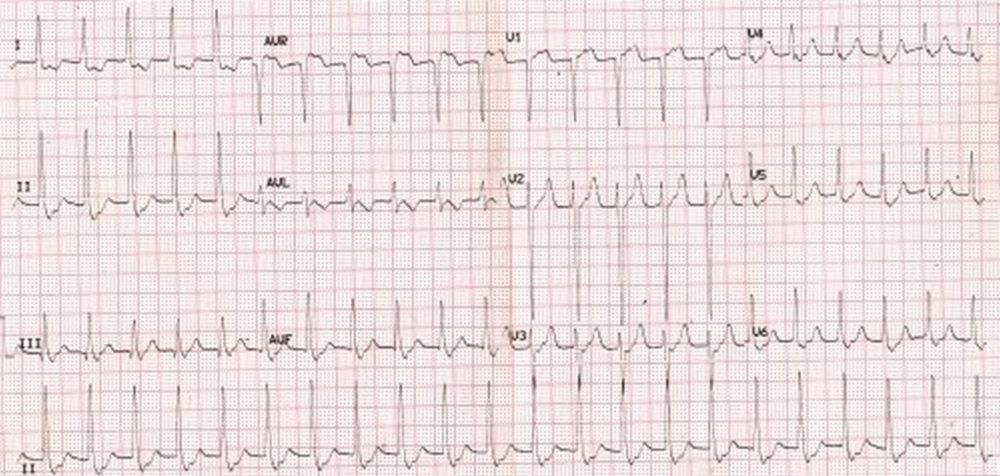
Supraventricular tachycardia with aberrant conduction indicated by right bundle branch block pattern (terminal slurred R in V1 and terminal slurred S in lead I. Atrial flutter with 2:1 conduction is an important differential diagnosis for this ECG. Vagal manoeuvres can be used to slow the AV nodal conduction and alter the conduction ratio to bring out hidden flutter waves within the QRS complexes if any. In case of true supraventricular tachycardia, these manoeuvres may terminate the tachycardia. Same is true of intravenous adenosine, which induces transient AV block, in a more predictable way. The prominent terminal R’ and S in this case are different from the tiny pseudo r’ and pseudo s due to retrograde P waves.
Classification of supraventricular tachycardias
Supraventricular tachycardias (SVT) can be classified into atrial and atrioventricular depending on the region of re-entry. It can also be divided into regular or irregular, with atrial fibrillation being the commonest form of irregular tachycardia with a supraventricular origin. The QRS complexes can be narrow or wide when there is aberrant ventricular conduction or pre-excitation. SVTs can also be divided into AV node dependent vs AV node independent. Another form of classification of SVT is into short RP (long PR) vs long RP (short PR) interval tachycardias.
Tachycardias with atrial circuit are sinus tachycardia, sinus node reentrant tachycardia, atrial tachycardia, multifocal atrial tachycardia, atrial flutter and atrial fibrillation. The different types of atrial flutter are typical (counterclockwise), reverse-typical (clockwise), left atrial, atypical and scar related atrial flutter. Upper loop reentry, lower loop reentry and figure of eight re-entry are other descriptions of the circuits in atrial flutter.
Tachycardias with atrioventricular circuits are atrioventricular nodal reentrant tachycardia (AVNRT), AV reentrant tachycardia (AVRT) and junctional ectopic tachycardia (JET).
AVNRTs themselves can be of three types: typical, atypical and the slow-slow variety. In the typical variety, anterograde conduction is over the slow pathway and retrograde conduction is over the fast pathway. Hence the initiating premature atrial complex will have a long PR interval. The RP interval is short (short RP tachycardia) in this variety, with PR>RP interval. P wave is either within the QRS or at the terminal portion of the QRS. These P waves manifest as pseudo S waves in inferior leads and pseudo R waves in V1. In atypical AVNRT, the opposite pattern of activation is seen so that RP is more than the PR interval (long RP tachycardia). In the rare slow-slow pathway tachycardia, the reentry occurs between two slow pathways.AVRTs can be divided into orthodromic and antidromic. In orthodromic AVRT, the anterograde conduction is through the AV node and the
QRS complex is narrow. Orthodromic AVRTs contribute about 90% of the AVRTs. Antidromic AVRT has the reverse pattern and the QRS is wide and bizarre.
JET is due to enhanced automaticity of the AV node and can manifest AV dissociation in the ECG with a narrow QRS. It can be congenital as well as acquired. It can occur in the setting of cardiac surgery and responds to cooling (induction of hypothermia).
Initiation and spontaneous termination of SVT
Usually it is difficult to document the initiation and spontaneous termination of an arrhythmia. This is because the arrhythmia is already there when the person presents to the emergency department. Termination is most often achieved by vagal maneuvers or by medication. If a monitor with recording facility has been deployed during this period, it is possible to get the tracings of termination. But many a time in an emergency setting, recording part is forgotten and only monitoring is done. Getting a record of initiation and termination gives useful insight into the mechanism of the tachycardia.

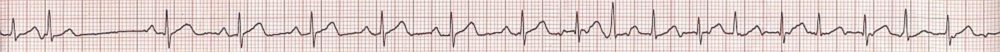
Monitor screenshot showing initiation of SVT by an SVPC. SVT: Supraventricular tachycardia; SVPC: Supraventricular premature complex. Sinus rhythm with normal PR interval is seen in the initial beats. A supraventricular ectopic (blue marker) is conducted with long PR interval as the fast pathway (AV nodal) has not recovered fully after conduction of the previous sinus beat. This leads to an echo beat (red marker). Supraventricular tachycardia (SVT) can be seen subsequently. The sudden increase in PR interval with a supraventricular ectopic beat is equivalent to the PR jump noted during EP (electrophysiology) study and indicates dual AV nodal physiology. PR jump of 50 milliseconds or more is considered indicative of dual AV nodal physiology.
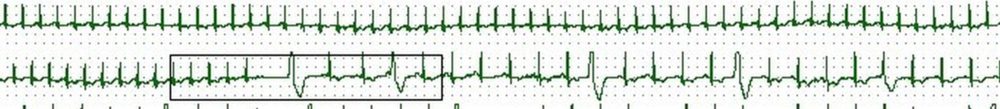
Monitor screenshot showing spontaneous conversion of SVT to sinus rhythm (SR). Initial 2 beats are part of the supraventricular tachycardia. Termination of tachycardia leads to a short pause and ventricular escape beat (wide QRS). This is followed by two narrow QRS beats, the P waves of which are not well seen (possibly of low amplitude). Next wide QRS complex is preceded by a P wave, indicating a late diastolic ventricular ectopic beat. The QRS width of this beat is lesser than that of the previous ventricular escape beat. Finally there is a good amplitude P wave followed by a narrow QRS after a normal PR interval, indicating sinus rhythm (SR).
Junctional rhythm
ECG manifestation of junctional rhythm has been conventionally divided into high junctional, mid junctional and low junctional. In high junctional rhythm inverted P waves occur before the QRS complex and there is a relatively short PR interval. Mid junctional rhythm is characterized by absence of P waves as the P waves are supposed to be simultaneous with QRS complexes. Low junctional rhythm manifests inverted P waves after the QRS complex, in the ST segment, with a short RP interval. In all these types the rate is around 40-60/min. Mid and low junctional rhythms are associated with regular cannon waves as the atrial contractions occur during ventricular systole when the AV valves are closed.
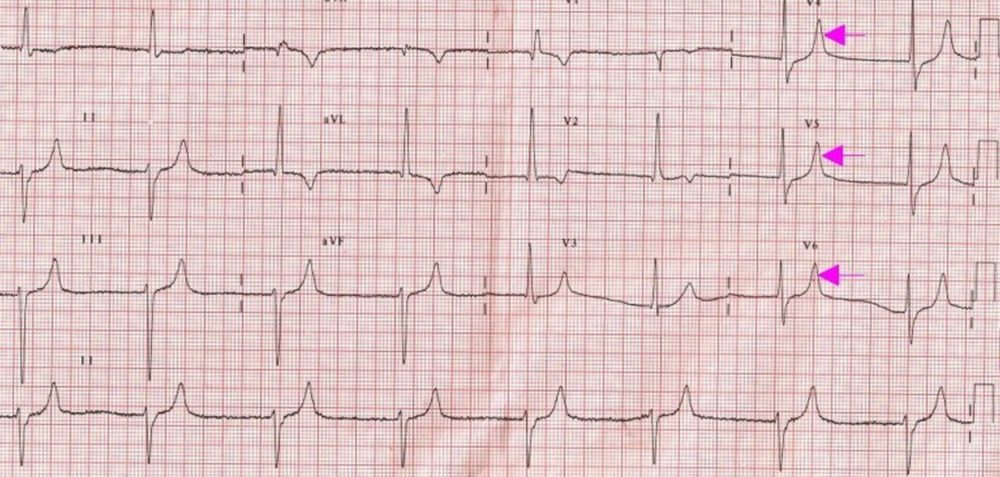
ECG shows a slow regular rhythm with a ventricular rate of around 43/min. Though there are some baseline artefacts, no definite P waves or fibrillary waves are seen. If the baseline artefacts are considered as fibrillary waves, then it has to be considered as atrial fibrillation with complete heart block and a junctional escape rhythm. If the baseline artefacts are ignored, it becomes a ‘mid junctional rhythm’. Alternate possibility in view of the tall peaked T waves (pink arrows) is an atrial paralysis with sinoventricular conduction in hyperkalemia.
Other findings in the ECG are left axis deviation with rS pattern in inferior leads suggesting left anterior hemiblock (LAHB) and qR pattern in V1 and a slurred S in V6 indicating right bundle branch block (RBBB). These two together constitute a bifascicular block. T wave is inverted in aVL. qR pattern in I and aVL also go with left anterior hemiblock. The difference in pattern between two QRS complexes in V1 is difficult to explain.
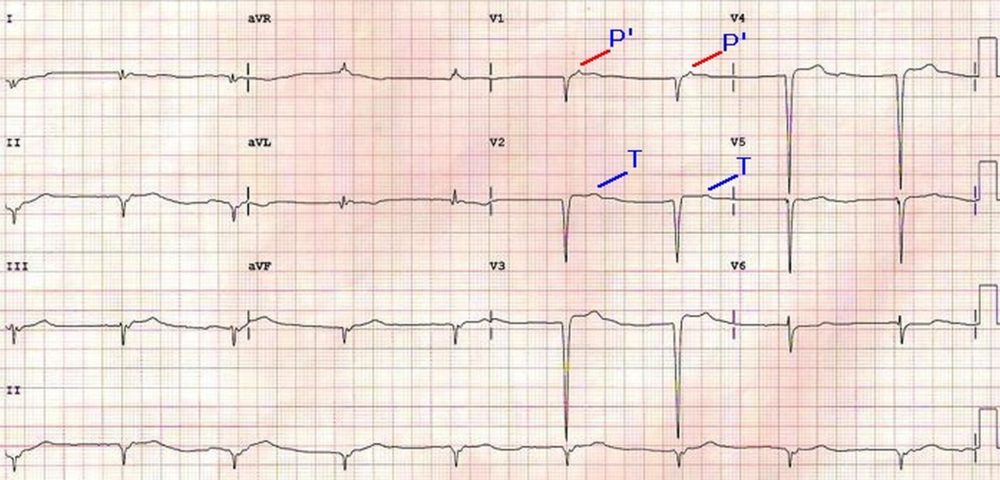
ECG shown below illustrates junctional rhythm with retrograde P waves (P’). P’ waves are seen on the ST segment in V1, preceding the T waves which are better seen in V2 than V1 and hence marked in V2 (T). QS complexes are noted in inferior and anterior leads indicating old anterior and inferior wall infarctions. The QRS complexes are not preceded by antegrade P waves. Retrograde P waves in the ST segment will make this a ‘low junctional rhythm’.
Low atrial rhythm
Low atrial rhythm manifests with inverted P waves in inferior leads. It may be seen in sinus venosus atrial septal defect.
Low atrial rhythm has been reported in acute amlodipine intoxication [1]. A rare autosomal dominant disorder in four generations of a family with congenital heart diseases (atrial septal defect, tetralogy of Fallot and persistent left superior vena cava) and low atrial rhythm has also been documented recently [2].
References
- Miranda CH, Xavier L, Fiorante F, Misiara GP, Guimarães EG, Galli AM, Pazin-Filho A, de Carvalho Borges M. Cardiac rhythm disturbances associated with amlodipine acute intoxication. Cardiovasc Toxicol. 2012 Dec;12(4):359-62.
- van de Meerakker JB, van Engelen K, Mathijssen IB, Lekanne dit Deprez RH, Lam J, Wilde AA, Baars MJ, Mannens MM, Mulder BJ, Moorman AF, Postma AV.Epub 2011 Mar 9. A novel autosomal dominant condition consisting of congenital heart defects and low atrial rhythm maps to chromosome 9q. Eur J Hum Genet. 2011 Jul;19(7):820-6.
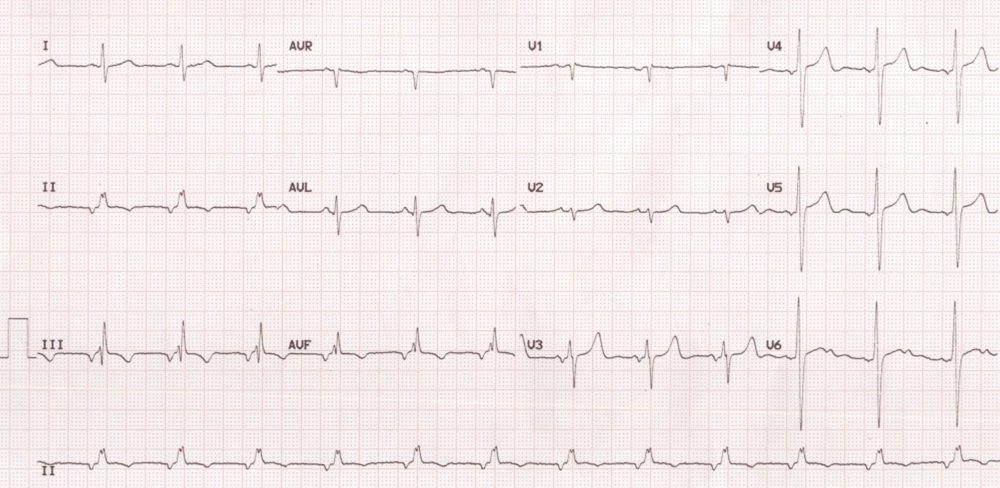
This ECG shows inverted P waves in inferior leads (II, III and aVF). This indicates that the atrial activation is spreading from below upwards. It is suggestive of a focus either in the low atrium or high junction. But the rate of around 75/min indicates the possibility of low atrial than high junctional rhythm. There is notching of the QRS complex in the inferior leads which suggest the crochetage sign in atrial septal defect. Low atrial rhythm can occur with sinus venosus atrial septal defect as the sinus node may be defective so that alternate focus arising in the low atrium gives the dominant rhythm. The PR interval is also shorter in low junctional and low atrial rhythm, more in the former than in the latter, as the conduction time needed to reach the ventricle is lower in the former.
Multifocal atrial tachycardia
Multifocal atrial tachycardia tachycardia can be defined as the occurrence of 3 more different morphologies of P waves at a rate more than 100/min. Multifocal atrial tachycardia is sometimes called as chaotic atrial rhythm because of the variability in atrial activity. Multifocal atrial tachycardia (MAT) can occur in those with chronic obstructive lung disease [1]. Ikaria study which evaluated the natural history of multifocal atrial rhythms in an elderly outpatient population showed that these rhythms are not associated with excess mortality in the elderly as in multifocal atrial tachycardias of hospitalised patients [2]. The study also showed that multifocal atrial rhythms have a high prevalence in the elderly, about 6%, with much higher prevalence in those above ninety years, about (15%).
Reference
- Goudis CA, Konstantinidis AK, Ntalas IV, Korantzopoulos P. Electrocardiographic abnormalities and cardiac arrhythmias in chronic obstructive pulmonary disease. Int J Cardiol. 2015 Nov 15;199:264-73.
- Lazaros G, Chrysohoou C, Oikonomou E, Tsiachris D, Mazaris S, Venieri E, Zisimos K, Zaromytidou M, Kariori M, Kioufis S, Pitsavos C, Stefanadis C. The natural history of multifocal atrial rhythms in elderly outpatients: insights from the “Ikaria study”. Ann Noninvasive Electrocardiol. 2014 Sep;19(5):483-9.
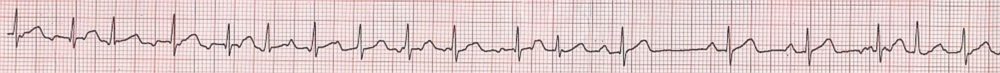
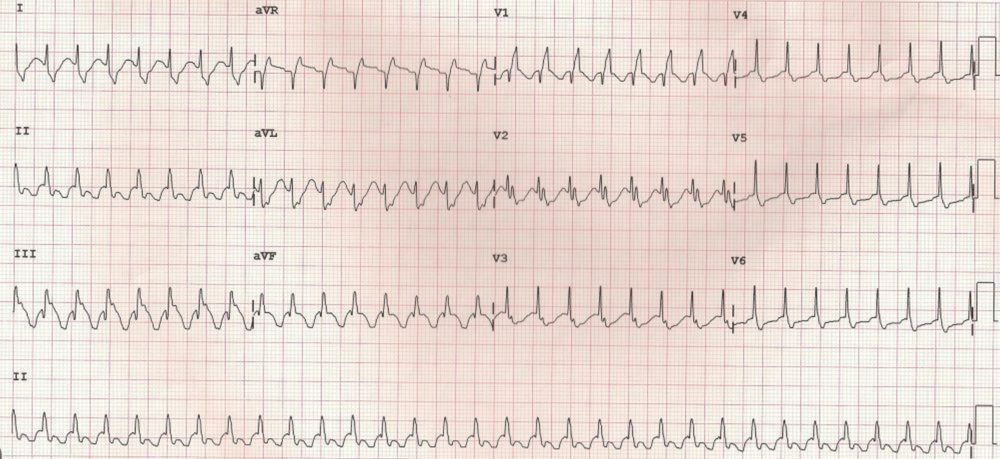
Multifocal atrial tachycardia is defined as three or more different types of P waves occurring at a rate more than 100 per minute. In the second rhythm strip there is a pause before the onset of sinus rhythm after the tachycardia terminates. This could be due to down regulation of the If current (funny current or pacemaker current) in the sinus node due to the tachycardia or due to a block atrial ectopic beat which is not very evident as it is superimposed on the T wave.
Multifocal atrial tachycardia and blocked atrial ectopic beat: Sinus rhythm is seen in the middle portion, while tachycardia is seen at both ends. Following the fourth beat in the rhythm strip, there is a pause due to a non-conducted atrial ectopic beat (blocked atrial ectopic).