Ventricular ectopic beats
Ventricular ectopic beats are also known as ventricular premature beats or complexes (VPB or VPC, sometimes PVC – premature ventricular complexes). They originate mostly due to reentrant circuits within the ventricles, but could also be due to triggered activity. Ventricular premature beats are easily recognized on the ECG by their wide bizarre QRS complexes, not preceded by a P wave. Secondary ST-T changes in the form of ST depression and T wave inversion when the QRS is dominantly positive are also seen. VPC is usually followed by a full compensatory pause, meaning that the interval between the previous sinus beat and the next sinus beat will be exactly double that of the sinus cycle length. This is because the VPC does not reset sinus cycle unlike the supraventricular ectopic which gets conducted to the sinus note earlier and resets the sinus cycle.
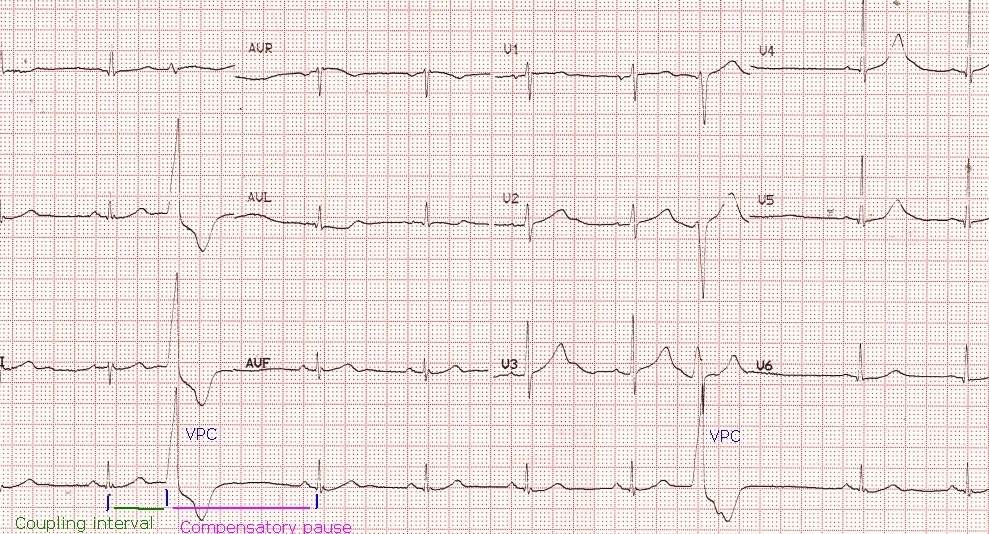
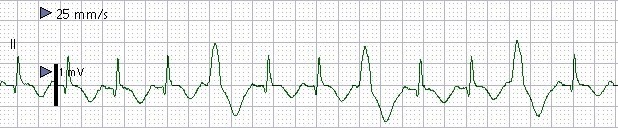
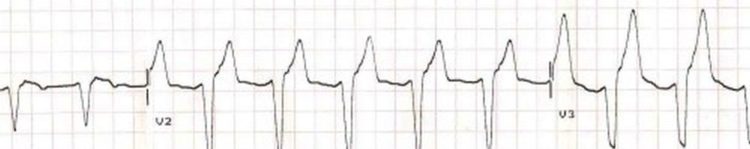
Basic rhythm in the ECG is sinus rhythm at around 60/min. There are two wide QRS complexes seen in lead II rhythm strip. Both of them are of similar morphology, hence they are called monomorphic VPC. Monomorphic VPCs are usually unifocal and have same coupling interval. Coupling interval is the interval between the onset of the previous normal QRS complex and the ectopic QRS complex. Ventricular ectopic is identified by the absence of preceding P wave, bizarre wide QRS and secondary ST-T changes. It is usually followed by a full compensatory pause, meaning that the sum of the coupling interval and the compensatory pause will be equal to twice the regular sinus cycle length. Compensatory pause is the interval between the onset of the ventricular ectopic beat and the succeeding sinus beat. The full compensatory pause is because the ventricular ectopic beat usually does not reset the sinus cycle. This is because the next sinus discharge would have already occurred before the ventricular ectopic impulse gets conducted up through the atrioventricular node with the usual delay.
Ventricular ectopics with different morphologies can be called polymorphic VPC. Polymorphic VPCs are more likely to lead on to more complex ventricular arrhythmias. They usually have different coupling intervals as they originate from different foci in the ventricle. Polymorphic VPCs were also called as multifocal VPCs. One classical type of polymorphic VPC is the bidirectional VPC with alternating QRS complexes being positive and negative. Bidirectional VPCs are the forerunners of bidirectional ventricular tachycardia, which is one of the types of polymorphic ventricular tachycardia. Monomorphic VPC usually lead on to monomorphic ventricular tachycardia. VPCs with short coupling interval are more likely to precipitate ventricular tachycardia or fibrillation. When the R wave of a VPC falls on the T wave of the previous cycle, it is known as R on T phenomenon, which is considered to be a forerunner of ventricular fibrillation. This is because the initial part of the descending limb of T wave is the most vulnerable phase in the electrical cycle, which is more prone for arrhythmia. That is why T wave shock is used to induce ventricular fibrillation while testing an implantable cardioverter defibrillator – a device used to automatically detect and treat dangerous arrhythmias.
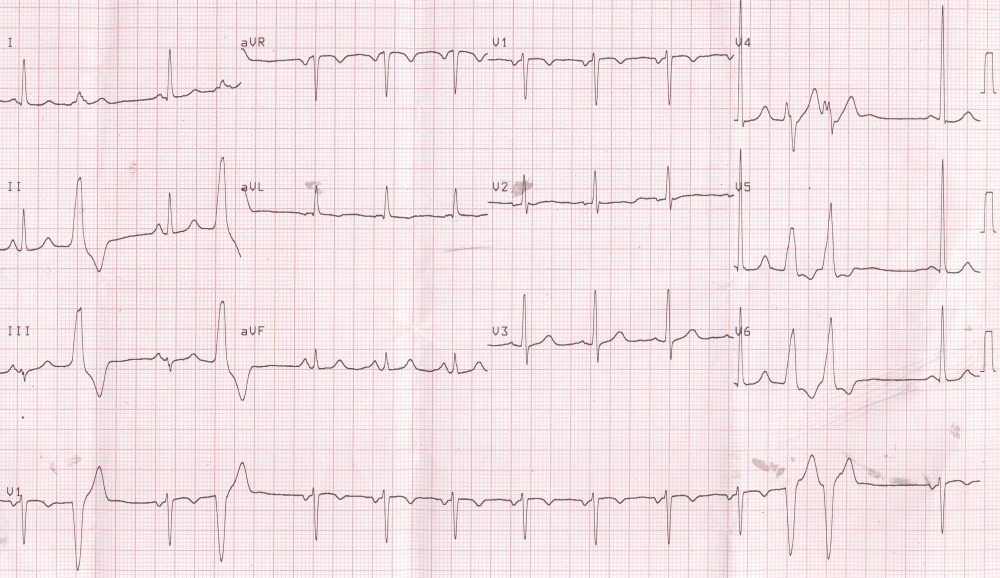
Initial two VPCs are isolated while the last two occur in rapid sequence as a couplet. VPC couplets may be a forerunner of ventricular tachycardia. Isolated VPCs and the couplet are followed by a compensatory pause. All the VPCs have same morphology (monomorphic) indicating the same focus of origin (unifocal). Unifocal VPCs usually have the same coupling interval.
Complex ventricular ectopy
Complex ventricular ectopy is the occurrence of multiple bizarre QRS complexes without preceding P waves and having different morphologies and coupling intervals. Since they have different morphologies, they are unlikely to be amenable for radiofrequency catheter ablation as they originate from multiple foci. Complex ventricular ectopy occurring frequently over a long period of the order of a decade can predispose to tachycardiomyopathy. Tachycardiomyopathy is a condition in which long standing fast heart rate predisposes to left ventricular dysfunction. The dyssynchrony of the left ventricular contraction due to altered sequence of activity during ventricular ectopy is an important contributor to left ventricular dysfunction. On the other hand complex ventricular ectopy can be an association of familial dilated cardiomyopathy as well.
Ventricular bigeminy, trigeminy and quadrigeminy
When each sinus beat is followed by a VPC, it is called ventricular bigeminy. It is associated with pulsus bigeminus. In the yesteryears when digoxin usage was high, ventricular bigeminy used to be an important manifestation of digoxin toxicity to look for. Bidirectional VPC and ventricular tachycardia in which consecutive VPC had QRS complexes of opposite polarity, were considered classical features of digitoxicity. When every two consecutive sinus beats are followed by a VPC it is called ventricular trigeminy. Similarly, when three consecutive sinus beats are followed by a VPC, it is called ventricular quadrigeminy. These are associated with corresponding changes in the pulse. The pulse of a VPC is usually of low volume so that sometimes it may be hardly felt. In some cases of ventricular bigeminy, this may lead to miscounting of pulse rate and the pulse rate will be counted as half the heart rate and bradycardia alert issued by the ward staff. The pulse following the compensatory pause has a higher volume because of better ventricular filling during the pause and enhanced inotropy.
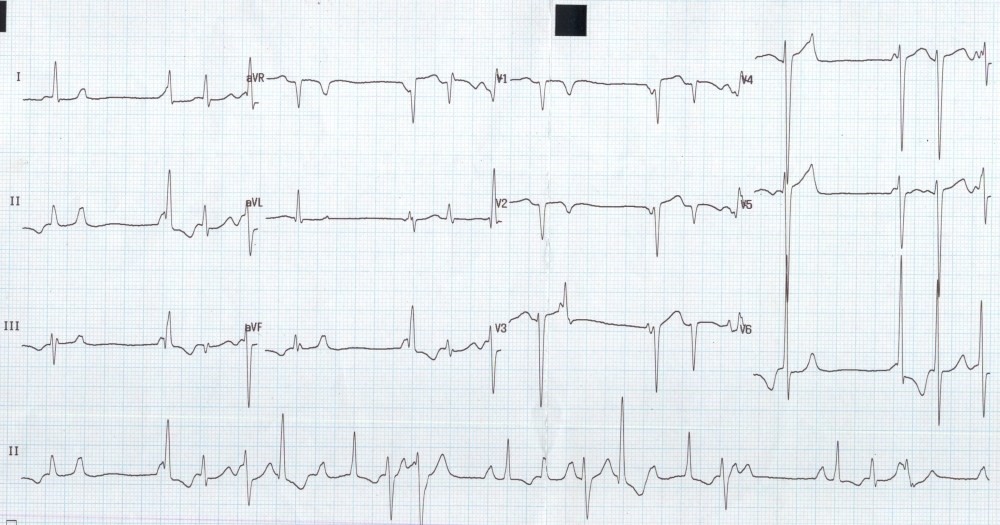
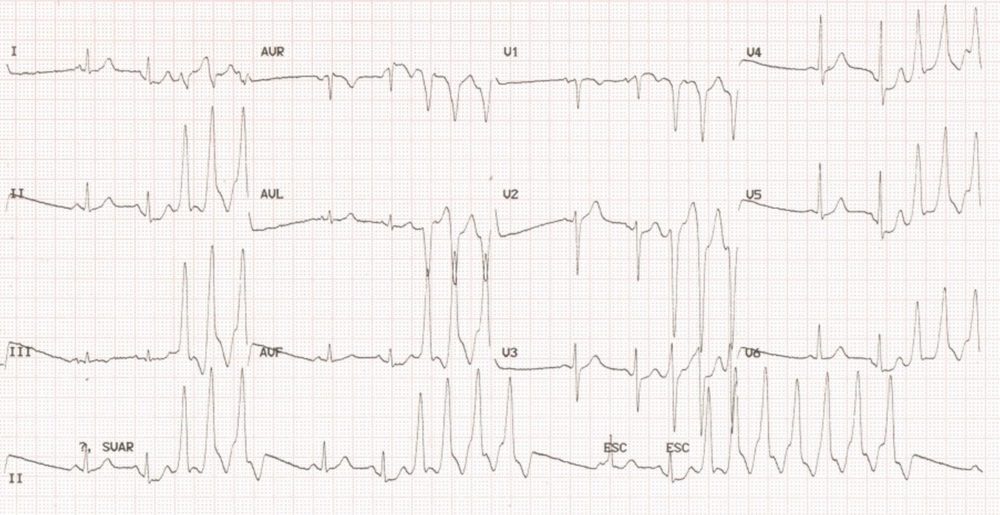
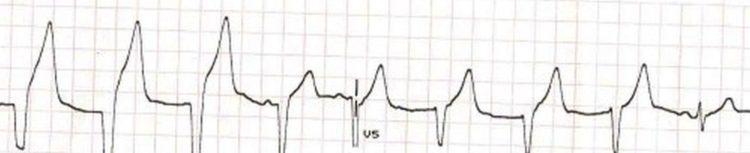
Multiple wide bizarre QRS complexes without preceding P waves are ventricular ectopic beats. Since they have different morphologies, they are called polymorphic VPC. Some of the couplets are seen to be bidirectional (bidirectional VPC), while others are unidirectional. In addition, there are QS complexes in V1 and V2 with a slightly coved ST segment and T wave inversion, reminiscent of an old myocardial infarction. Bidirectional VPC and bidirectional ventricular tachycardia can be seen in digoxin toxicity, Anderson-Tawil syndrome (congenital long QT syndrome 7), catecholaminergic polymorphic ventricular tachycardia, myocarditis, myocardial infarction and metastatic cardiac tumours
Reference
- Chakraborty P, Kaul B, Mandal K, Isser HS, Bansal S, Subramanian A. Bidirectional ventricular tachycardia of unusual etiology. Indian Pacing Electrophysiol J. 2016 Feb 23;15(6):296-9).
Ventricular ectopic bigeminy: Clinical findings will be pulsus bigeminus and intermittent cannon waves as alternate P waves are falling on the T waves. When P waves fall on the latter part of QRS, ST segment or T waves, cannon waves can be expected as QT interval roughly represents the electrical systole of the ventricle. (Diastole ends and systole starts at the peak of R wave). In the tracing, P waves are seen as distortions in the contour of the T wave of the ectopic beat. The distortion is exactly midway between the preceding and succeeding P waves of the sinus beats (narrow QRS). Ventricular ectopics are characterised by wide bizarre complexes which are premature and not preceded by P wave. The ventricular ectopic beats are followed by a full compensatory pause meaning that the sum of the coupling interval (interval from the onset of the previous QRS to the onset of the ectopic QRS) and the compensatory pause (the next RR interval) will be exactly twice that of the RR interval of sinus beats. The exact compensatory pause is because the sinus cycle is not reset by the ventricular beat as it finds the retrograde path to the sinus node refractory. Sometimes the retrograde conduction to the AV node produces a prolongation of conduction of the next sinus beat manifesting as a prolongation of the next PR interval (not present in this ECG). This is a manifestation of concealed retrograde conduction.
Monitor screenshot showing three ventricular premature complexes (VPC) occurring in a trigeminal sequence (two sinus beats followed by a ventricular ectopic beat – ventricular trigeminy or VPC Trigeminy). Ventricular premature complexes are identified as being premature complexes with a wide bizarre QRS complexes having no preceding P waves. In this case the VPCs are not so premature with the coupling interval from the previous sinus beat being about 400 ms and that from the VPC to the subsequent sinus beat being about 560 ms. The standardization of 1 mV to one cm on the Y-axis and a sweep speed of 25 mm/s on the X-axis are displayed in the tracing. Each VPC is followed by a fully compensated compensatory pause. In this case the pauses are not very prominent because the usual heart rate itself is high and the difference between the coupling interval and the compensatory pause is small. Coupling interval is the interval from the onset of the previous sinus beat to the onset of the ectopic beat. Compensatory pause is the pause after the ventricular ectopic beat. The sum of the coupling interval and the compensatory pause will be twice the basic sinus cycle length.
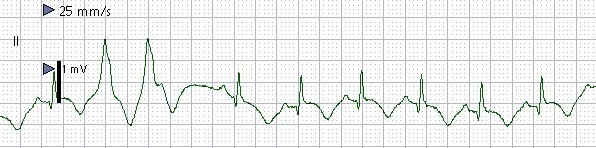
Monitor screenshot showing ventricular premature complexes in a couplet form (VPC couplet), with no preceding sinus beat in between. The two VPCs (second and third complexes) are seen as wide monophasic QRS complexes with inverted T waves. they occur in quick succession with a cycle length of 400 milliseconds which would correspond to a ventricular rate of 150/min should more VPCs occur in sequence to form a ventricular tachycardia. A compensatory pause is seen after the second VPC. The basic sinus cycle length is near 600 ms corresponding to a rate of around 100 per minute. Sweep speed of the monitor is shown as 25 mm/s and the standardization at 1 mV to a cm. Sinus beats also show T wave inversion, possibly due to underlying primary T wave change due to ischemia / infarction, which has caused the myocardial irritability in the form of VPC couplet. Though VPC couplets themselves are harmless, they could be a forerunner of ventricular tachycardia, which needs to be anticipated and treated if it occurs.
Ventricular tachycardia
Three or more ventricular complexes (wide QRS) occurring at a rate more than 100 per minute is taken as ventricular tachycardia (VT). Ventricular tachycardia is one of the two common, potentially life threatening serious ventricular arrhythmias, latter being ventricular fibrillation. Ventricular tachycardia lasting more than 30 seconds or requiring termination prior to that due to hemodynamic compromise is called sustained ventricular tachycardia. Shorter spells of ventricular tachycardia are called non sustained ventricular tachycardia (NSVT). If all the QRS complexes in a VT have same morphology, then it is called monomorphic ventricular tachycardia (MMVT). If the QRS morphology is varying, it is called polymorphic ventricular tachycardia (PMVT). The classical type of polymorphic VT associated with QT interval prolongation is called torsades des pointes, because it resembles ‘twisting of points’ in an ECG strip, with QRS morphology transitioning slowly from positive to negative and back. Torsades des pointes is an important toxicity of many drugs which prolong the QT interval. Hence it has been made mandatory to test the effect on QT interval of any new drug before approval is granted by the national drug control agency. Torsades can also occur in the setting of myocardial ischemia, complete heart block and electrolyte imbalances like hypokalemia and hypomagnesemia.
NSVT – salvo of ventricular premature complexes
Even though three ventricular ectopics in succession with a rate above 100/min qualifies for calling it a non sustained ventricular tachycardia run, it is often called a salvo of ventricular ectopics.
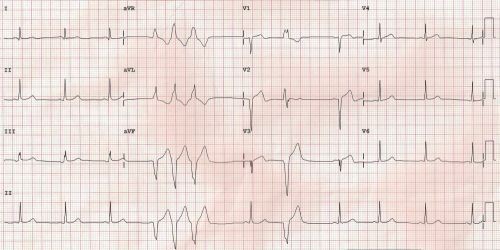
Salvo of ventricular premature complexes: Leads V1- V3 shows a single wide QRS complex with an M shaped pattern in V1 suggesting an origin from the left ventricle. The transition of the QRS complex of the VPC (ventricular premature complex) from positive to negative occurs early, in lead V2. Leads V3-V6 has not captured any VPC. There is a salvo of three wide QRS complexes in aVR, aVL and aVF. The original meaning of the word salvo is a series of shots fired in rapid sequence from a gun or simultaneously from multiple guns. Here the wide QRS complexes occur at a rapid rate nearing 150 per minute. No wide QRS complexes are seen in leads I and III. Lead II shows wide QRS salvo in the rhythm strip. The axis of the wide QRS salvo is superior, as they are negative in leads II and aVF. This would suggest a focus in the lower part of the ventricle with activation spreading upwards.
Ventricular ectopic beats originating from the right ventricular outflow tract (RVOT) is one of the commonest forms of benign ventricular ectopy. But at times RVOT can be the origin of a ventricular tachycardia (VT) which could be either paroxysms of nonsustained ventricular tachycardia (NSVT) as seen above or sustained ventricular tachycardia. RVOT VT can be induced by exercise and has a left bundle branch block morphology (wide QRS which is negative in V1 and positive in V6) with inferior axis (positive in leads II, III, aVF).

ECG showing VT occurring during an exercise test. The initiating beat is a ventricular ectopic beat with R on T phenomenon. It is a monomorphic VT with QRS negative in V1 and positive in II and V5 suggestive of RVOT VT.
Polymorphic ventricular tachycardia often occurs in recurrent episodes and usually does not need direct current cardioversion. Rather it needs treatment for the cause which could be intravenous magnesium or temporary pacing. If there is associated hypokalemia, it has to be corrected. Any offending drug has to be withdrawn in case of drug induced torsades.
Sustained monomorphic ventricular tachycardia can be treated with intravenous amiodarone or lignocaine. Those not responding to medication or in case of hemodynamic compromise, rapid direct current cardioversion is needed. Recurrent episodes of monomorphic ventricular tachycardia in spite of medications may need more definitive treatment modalities like radiofrequency catheter ablation and implantation of a cardioverter defibrillator. Stellate ganglion ablation or surgical removal is another option for recurrent monomorphic ventricular tachycardia.
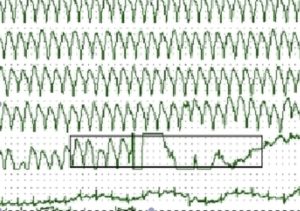
Monitor screen shot showing ventricular tachycardia and restoration of sinus rhythm following cardioversion with a direct current shock. Shock can be seen as the vertical line which terminates the tachycardia within the box. Sinus rhythm resumes within a short while. Sometimes there is a short period of bradycardia after a shock.

Monitor screenshot showing frequent runs of nonsustained ventricular tachycardia. Inset shows a short segment in more detail. dissociated P waves are seen very well indicating the ventricular origin of the tachycardia. P waves are seen before the 6th and the 11th QRS complexes, with different PR intervals, indicated that they are dissociated P waves. Here the P waves are of sinus origin and do not get conducted to the ventricles because ventricle is already activated by a faster ventricular rhythm. Retrograde conduction from the ventricle into the AV conduction and antegrade conduction from the sinus node gets cancelled off and this a form of ‘interference AV dissociation’.
Idiopathic Fascicular Ventricular Tachycardia (Belhassen’s VT)
Belhassen’s VT is idiopathic fascicular ventricular tachycardia originating from the left posterior fascicle. It is responsive to verapamil and is an ablatable VT. It is also known as posterior fascicular tachycardia. Belhassen and associates described a ventricular tachycardia responding to verapamil [1], unlike the usual ventricular tachycardias which respond to lignocaine. It may be noted that verapamil is conventionally a drug used for treatment of supraventricular rather than ventricular tachycardia. Even though other authors had reported on ventricular tachycardias with relatively narrow QRS complex originating from the posterior fascicle [2], it was Belhassen and colleagues who suggested this form of ventricular tachycardia as a separate entity [3].
ECG patterns in fascicular ventricular tachycardia
Classical ECG pattern in Belhassen’s VT is right bundle branch block pattern with left axis deviation as it originates from the left posterior fascicle. Tachycardia originating from the left anterior fascicle has right bundle branch block pattern with right axis deviation and that originating from the left septal fascicle has right bundle branch block pattern with normal axis [4].
References
- Belhassen B, Rotmensch HH, Laniado S. Response of recurrent sustained ventricular tachycardia to verapamil. Br Heart J. 1981 Dec; 46(6): 679-82.
- Cohen HC, Gozo EG Jr, Pick A. Ventricular tachycardia with narrow QRS complexes (left posterior fascicular tachycardia). Circulation. 1972 May; 45(5): 1035-43.
- Belhassen B, Shapira I, Pelleg A, Copperman I, Kauli N, Laniado S. Idiopathic recurrent sustained ventricular tachycardia responsive to verapamil: an ECG-electrophysiologic entity. Am Heart J. 1984 Oct; 108(4 Pt 1): 1034-7.
- Francis J, Venugopal K, Khadar SA, Sudhayakumar N, Gupta AK. Idiopathic Fascicular Ventricular Tachycardia. Indian Pacing Electrophysiol. J. 2004;4(3):98-103.
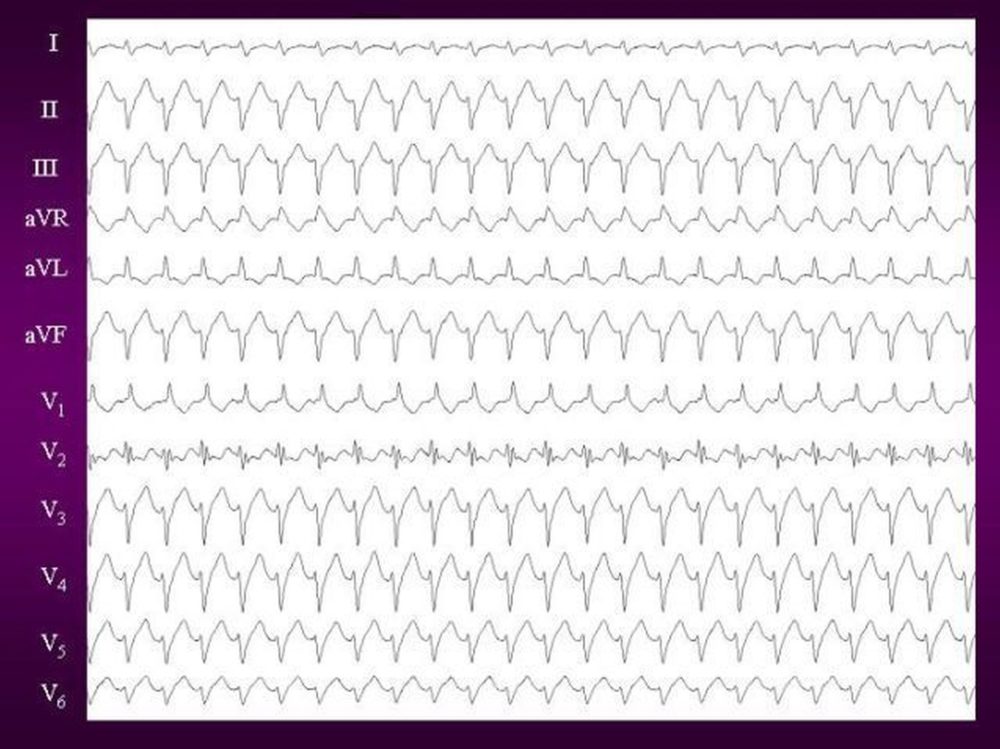
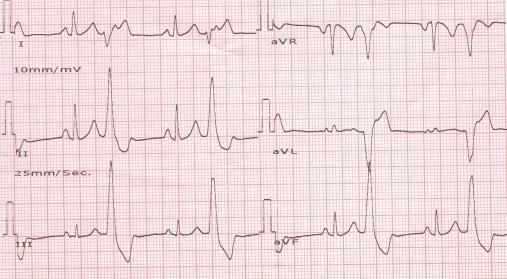
12 lead ECG of Idiopathic Fascicular Ventricular Tachycardia showing classical right bundle branch block (RBBB) pattern with leftward axis morphology suggestive of posterior fascicular origin. (Courtesy: Francis J et al [Reference 4 above]).
Ventricular fibrillation
Ventricular fibrillation (VF) is a life threatening arrhythmia, which leads to death unless promptly corrected by electrical defibrillation (direct current or DC shock). In VF, the electrical activity is so disorganized that no ventricular contraction is possible and ventricle remains still in a state of cardiac arrest.
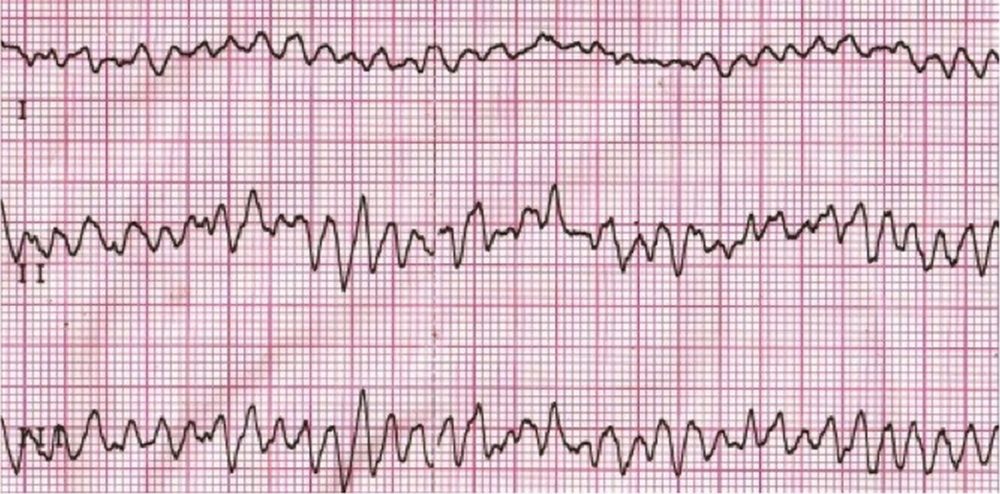
Ventricular fibrillation (VF) is recognized on the electrocardiogram (ECG) as a highly disorganized electrical activity. Each wave has a different morphology. When multiple simultaneous leads are available as in this case, it can be seen that the morphology is different between the leads as well. Here it is coarse VF.
As time passes after the onset of ventricular fibrillation, the initially coarse ventricular fibrillation degenerates into fine ventricular fibrillation. If you are noting fine ventricular fibrillation on the monitor in a case of cardiac arrest, it usually means that some time has passed after the onset of ventricular fibrillation. Fine ventricular fibrillation is more difficult to convert electrically by defibrillation. Often a few cycles of cardiopulmonary resuscitation (CPR) and administration of adrenaline, may convert fine VF back to coarse VF and make it more amenable to defibrillation. Usually fine VF indicates underlying metabolic acidosis, which improves with CPR.
Accelerated idioventricular rhythm
Accelerated idioventricular rhythm (AIVR) is spontaneous rhythm originating from the ventricle which is faster than the usual idioventricular rhythm in complete heart block which has a rate of around 20 – 40/min. AIVR typically has a rate just above 100/min, but is slower than the usual ventricular tachycardia. It is sometimes called as slow VT. AIVR is considered as a classical reperfusion arrhythmia which occurs after successful reperfusion of a coronary occlusion, either by thrombolysis or percutaneous coronary intervention. Usually it is a self-limited arrhythmia and needs no treatment.
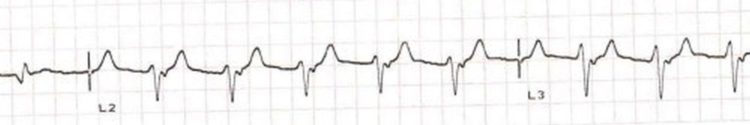
Accelerated idioventricular rhythm (AIVR) with regular retrograde P waves. Retrograde P waves are seen just after the QRS in L2 and L3. The P waves are not that evident in L1. The retrograde atrial activation will result in regular cannon waves in the jugular venous pulse. Even though the QRS complex is almost 120 ms in width, at one look it may appear to be not that wide and the AIVR can be missed.
In this tracing of AIVR, the wide QRS is quite evident. The P waves are not very evident, though careful examination will reveal the slight notching of the upstroke of the T waves, which are the hidden P waves. Looking for hidden P waves is always a challenging part of arrhythmia analysis. Presence of hidden P waves which are dissociated from QRS complexes indicate a ventricular origin of the rhythm. Usually the hidden P waves are of sinus origin and they just overlap the ventricular rhythm. Occasionally hidden P waves could be due to retrograde conduction from the ventricular focus.
The fourth beat shows a P wave with reasonable PR interval and a QRS which is narrower than the initial three beats (of AIVR), suggesting that it is a fusion beat. Fusion beat is partly conducted beat (initial part) and partly ventricular ectopic beat (latter part). Fusion beat has a morphology intermediate between a fully conducted beat and an ectopic beat. The last beat is preceded by a P wave and has a narrow QRS indicating that it is a capture beat. Capture beat is a sinus beat occurring in between ventricular tachycardia beats (or within AIVR). Presence of capture beats and fusion beats confirm the ventricular origin of the focus in a wide QRS tachycardia (or rhythm).