Continued from Supraventricular Arrhythmia – Part 1
Atrial fibrillation
Atrial fibrillation (AF) is the most common sustained arrhythmia. AF can be recognized in the ECG with absence of organized atial activity (P waves) and the presence of fibrillary waves. AF can be either fine AF or coarse AF depending on the amplitude of fibrillary waves. Fibrillary waves of more than 1 mm (0.1 mV) amplitude is called coarse AF and indicates atrial enlargement. AF can occur acutely in situations of sympathetic overactivity or due to rapid dilatation of the atria due to ventricular dysfunction. Chronic atrial dilatation and fibrosis predisposes to persistent atrial fibrillation. In chronic AF there is electrical remodeling of the atria.
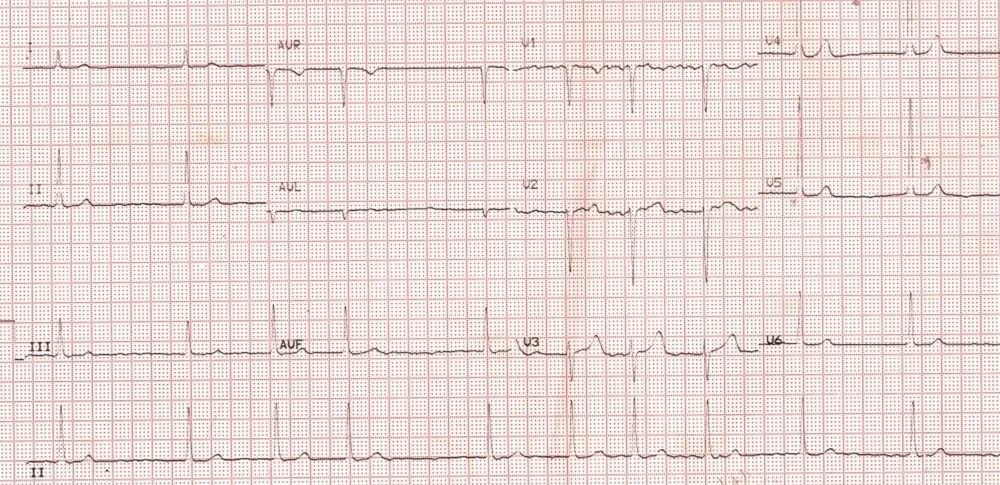
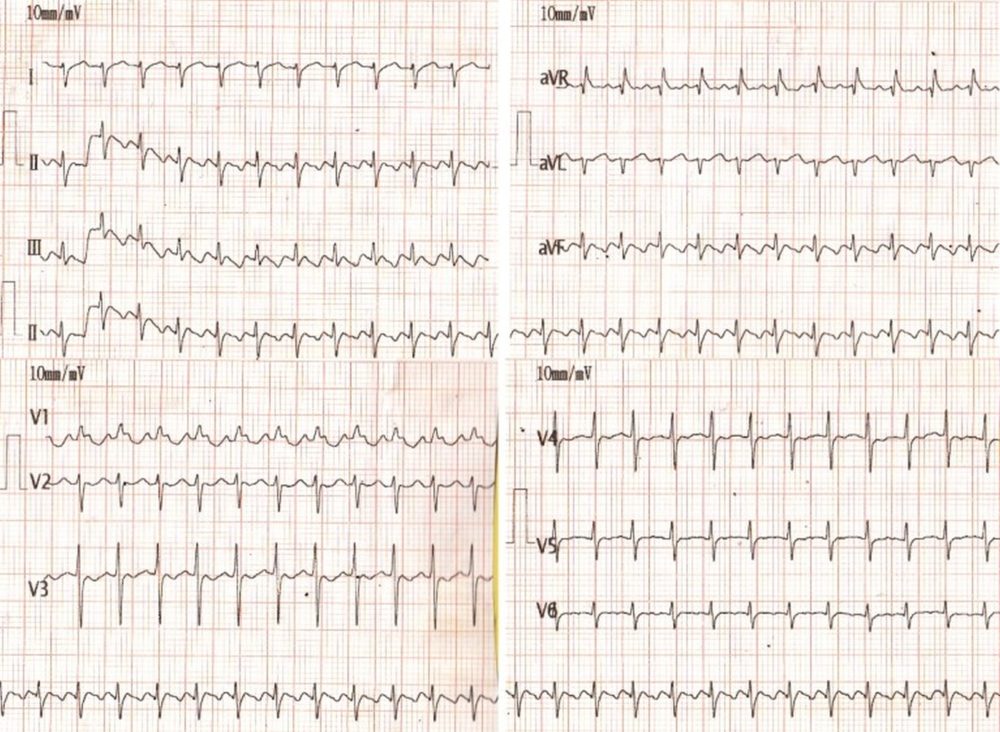
Atrial fibrillation with slow ventricular rate. Fine fibrillary waves are seen throughout the baseline, indicating fine atrial fibrillation
ECG showing atrial fibrillation with slow ventricular rate and left ventricular hypertrophy. Slow ventricular rate is due to suppression of the atrioventricular conduction either due to drugs or due to disease of the atrioventricular node. Left ventricular hypertrophy is manifest as tall R waves with ST segment depression in lateral leads. Digoxin effect could also contribute both slow rate and ST segment changes. The coarse fibrillary waves in V1 suggest possibility of a large atrium as in mitral stenosis. Fibrillary waves of more than 1 mm amplitude indicate atrial enlargement. Left ventricular hypertrophy indicates associated lesions like mitral regurgitation or aortic valve disease as left ventricular hypertrophy does not occur in isolated mitral stenosis.
Atrial fibrillation with aberrant ventricular conduction
Atrial fibrillation with aberrant ventricular conduction will present as wide QRS tachycardia resembling ventricular tachycardia. Aberrancy could be transient aberrancy occurring due to fast ventricular rate causing aberrant conduction in one of the bundle branches, usually the right bundle. Alternatively it could be pre-existing bundle branch block on top of which atrial fibrillation occurs. Yet another reason for wide QRS in atrial fibrillation is pre-excitation (WPW syndrome). In WPW syndrome with atrial fibrillation, ventricular rates can go very high due to simultaneous conduction through normal AV nodal pathway and the accessory pathway. Unlike the normal AV nodal pathway whose refractory period increases at fast rates, accessory pathway refractory period shortens at fast rates and can lead to dangerous ventricular rates, degenerating into ventricular fibrillation. Hence AF with WPW syndrome is often associated with hemodynamic compromise and indication for rapid electrical cardioversion. Shortest RR interval will be equal to the effective refractory period of accessory pathway.
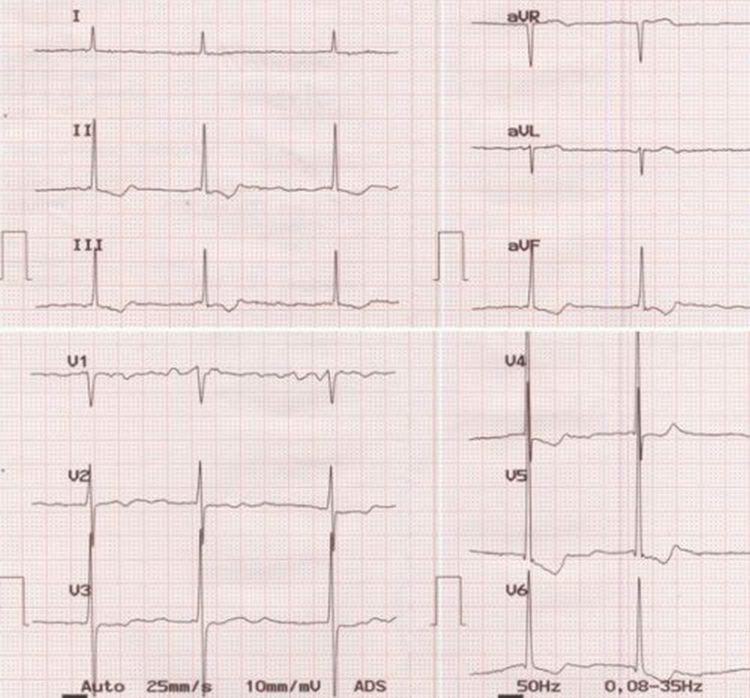
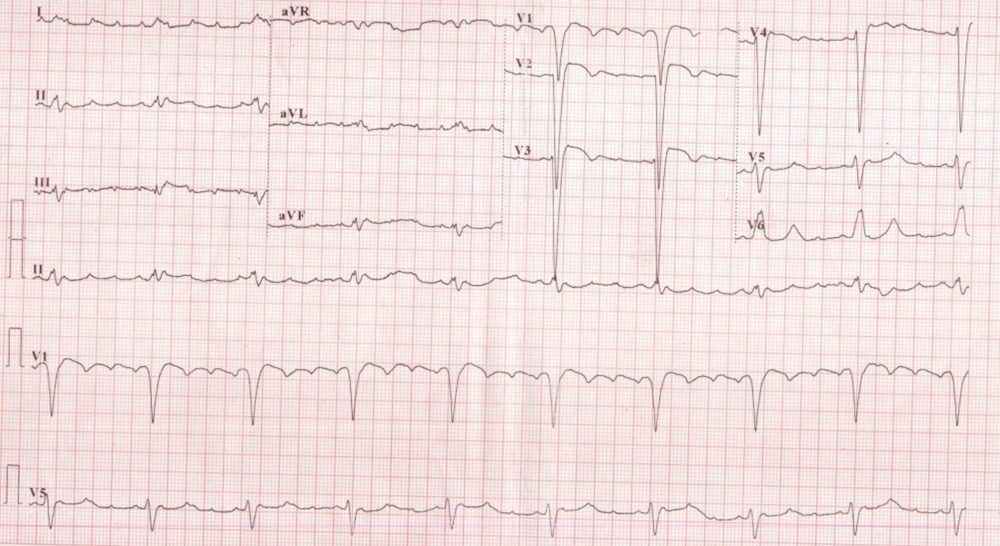
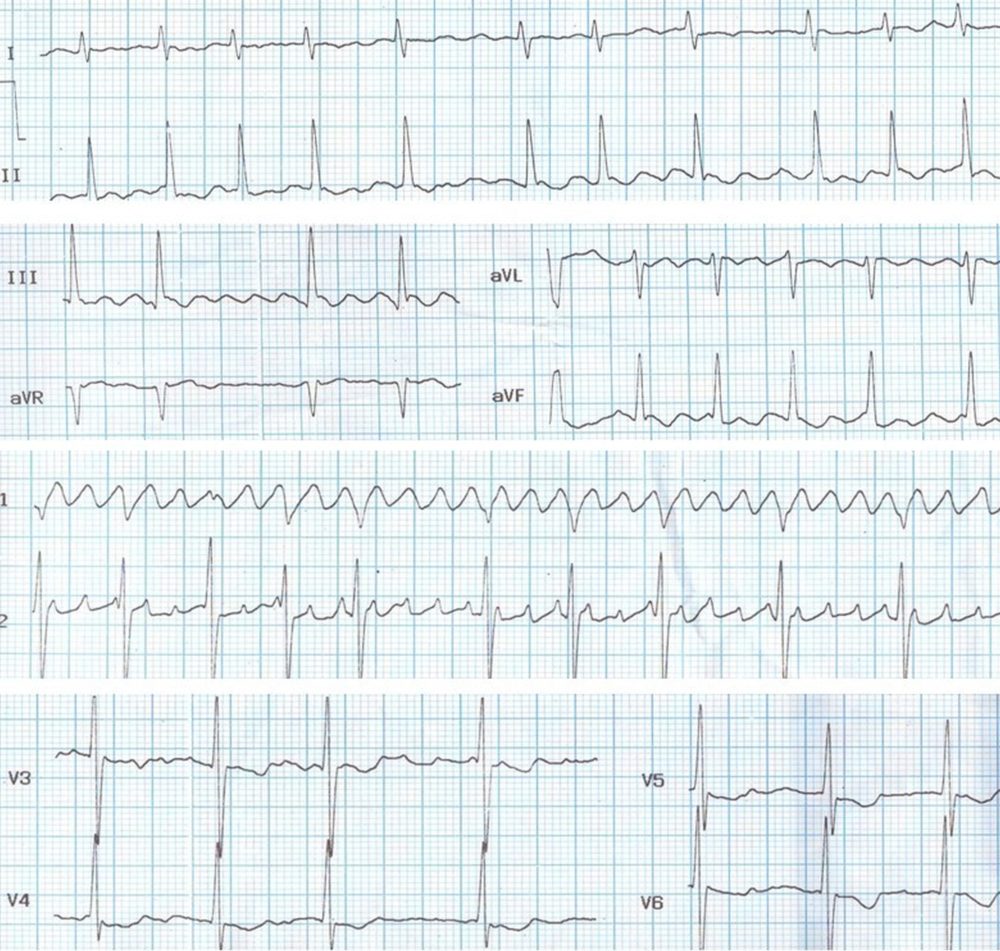
Atrial fibrillation with WPW syndrome causing a wide QRS tachycardia. High ventricular rates are possible because the refractory period of accessory pathway shortens with increase in rate. Usually this is mistaken for ventricular tachycardia in the emergency department and cardioverted because of almost invariable association of hemodynamic compromise. Close inspection of the ECG (often retrospectively, after cardioversion), shows the distinct variation in cycle length – over 50% difference between the shortest and longest RR intervals, indicating that the underlying rhythm is atrial fibrillation. Fibrillary waves of atrial fibrillation are seldom seen in this situation as it is fine atrial fibrillation in the absence of atrial enlargement. A good baseline to demonstrate fibrillary waves is also unlikely at such fast rates. In addition there is variation in QRS width (concertina effect) due to the varying degrees of pre-excitation for each QRS complex. These two features differentiate it from ventricular tachycardia. Moreover post conversion ECG will show classical features of WPW syndrome with short PR interval, slurred initial part of the QRS known as delta wave and secondary ST-T changes. This is why the dictum that we should always take a repeat ECG after treatment of any sustained cardiac arrhythmia.
Atrial Flutter
Typical atrial flutter manifests as sawtooth waves (F) in inferior leads. Usually the conduction ratio is 2:1 so that there will be double the number of flutter waves compared to QRS complexes. But alternate flutter waves are not evident, being masked by the overlying QRS complexes. When the conduction ratio is 3:1 or 4:1, the flutter waves become more evident. Carotid sinus compression can change the conduction ratio and make the flutter waves visible during continuous monitoring in an intensive care unit. Administration of adenosine has a similar effect and multiple sequential flutter waves can be visible during the transient atrioventricular block produced by adenosine.
Atrial flutter is often missed on an ECG because the alternate flutter waves are masked by the QRS complex. A high index of suspicion is needed to diligently look for flutter waves in a supraventricular tachycardia at a rate of around 150/minute which is the typical ventricular rate in an atrial flutter with 2:1 conduction. The typical atrial flutter rate is 300/minute and commonest conduction ratio is 2:1 so that ventricular rate is 150/minute.
Atrial flutter with inverted flutter waves in inferior leads is called typical atrial flutter. When the flutter waves are upright in inferior leads, it is called reverse typical flutter. Both these types are due to macro reentrant circuits within the right atrium and are dependent on a zone of slow conduction in the cavotricuspid isthmus. Typical flutter has an anti clockwise intra atrial reentrant circuit while the reverse typical flutter has a clockwise reentrant circuit. Both types can be cured by ablation in the region of cavotricuspid isthmus.
Atrial flutter being a macro reentrant arrhythmia, is the one which is most sensitive to direct current cardioversion. Low energy levels of the range of 25 Joules are sufficient to convert the flutter to sinus rhythm, though it may recur if the underlying cause is remaining untreated.
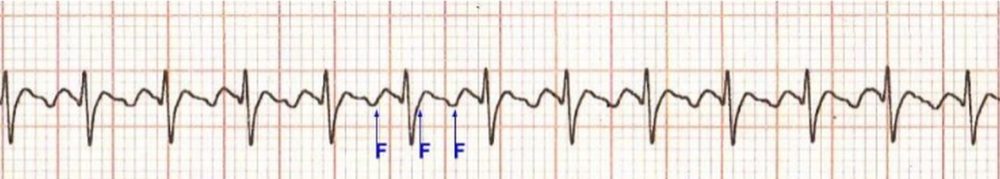
Atrial flutter with 2:1 conduction. Alternate flutter waves (F) are masked by the QRS complexes.
Neonatal atrial flutter with 2:1 conduction. The ‘saw tooth’ shaped flutter waves are seen well in the lead II rhythm strip. Atrial rate is about 400/min and ventricular rate around 200/min. Negative flutter waves in inferior leads suggest typical flutter.
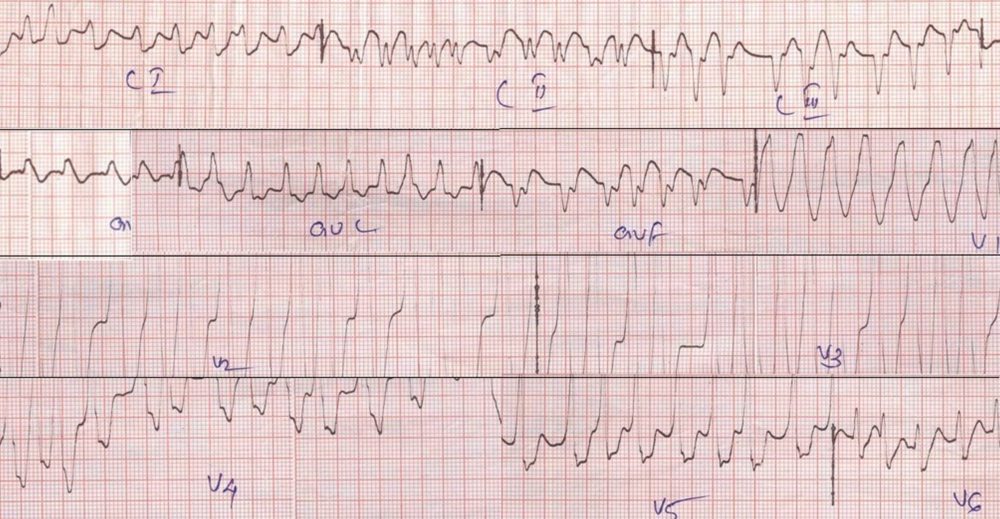
Atrial flutter with 4:1 conduction. Atrial rate is 272/min and ventricular rate 68/min. Flutter waves in inferior leads are upright suggesting reverse typical flutter. QRS complexes are wide and shows left bundle branch block pattern. T waves are concordant with QRS complexes in V6, but discordant in V5.
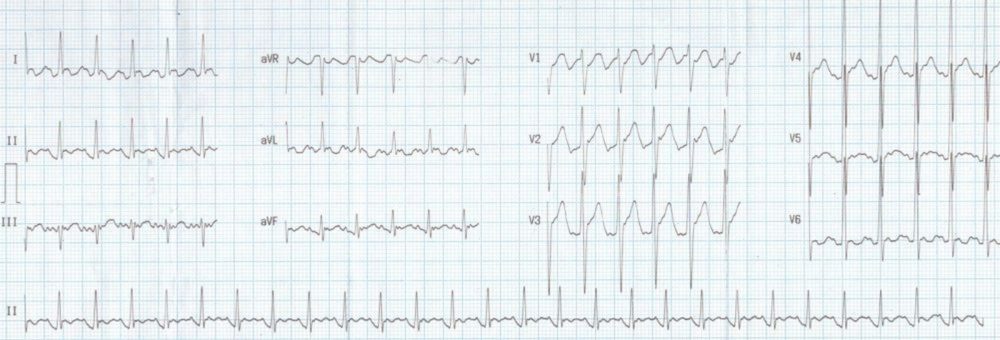
Atypical atrial flutter with 2:1 conduction: Flutter waves are seen well in leads I,aVL, aVR and V1. In inferior leads the flutter waves appear more like usual P waves. This is unusual because in typical flutter the flutter waves are seen well in inferior leads (compare the image below). Flutter waves are saw toothed in appearance and have a rate of 250 – 350 per minute. The ventricular rate may vary depending on the conduction ratio. One of the typical rates is 150 / minute with atrial rate of 300 per minute and 2:1 conduction. In fact when the ventricular rate is 150 / minute, one is supposed to look carefully for flutter waves in the ECG. Typical atrial flutter has positive P waves in V1 and negative P waves in V6, II, III and aVF. The reentrant circuit is counterclockwise, ascending up along the interatrial septum and descending down along the right atrial free wall. The reverse pattern is seen in reverse typical atrial flutter. In reverse typical atrial flutter, the P waves are negative in V1 and positive in V6, II, III and aVF. The reentrant circuit is clockwise, ascending up along the right atrial free wall and descending down the interatrial septum.
Atrial flutter in mitral stenosis
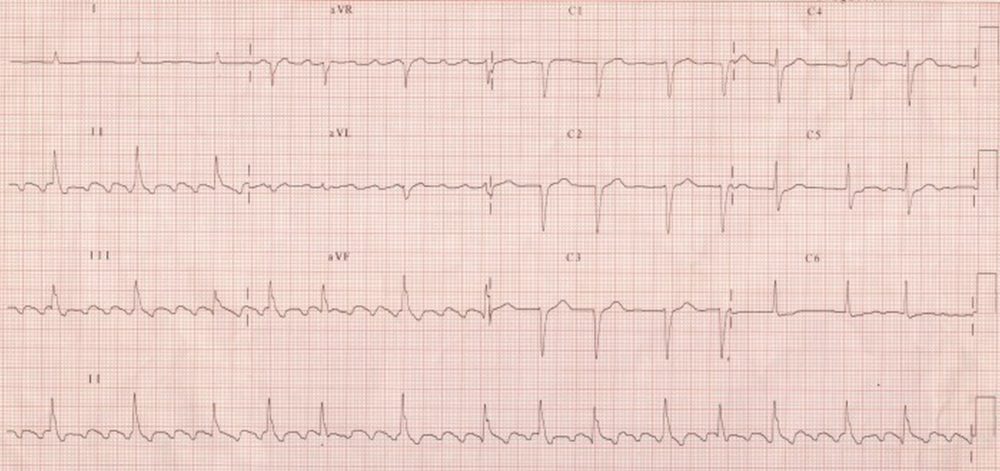
Atrial flutter is less common than atrial fibrillation in mitral stenosis. In the ECG shown below, the flutter waves are seen well in inferior leads and V1 has typical sawtooth waves while it is also seen in other leads. Such an organised flutter is rare in mitral stenosis. In most cases of mitral stenosis, the coarse fibrillary waves resemble flutter waves in some leads, but not in others. Such impure rhythms are sometimes called flutter-fibrillation, flitter or fib-flutter. In those cases the waves are irregular. In this ECG the waves are regular, suggesting true atrial flutter. The conduction ratio is varying so that the ventricular rate is irregular and resembling atrial fibrillation. The large atria in this case (both left and right atria as there is severe pulmonary arterial hypertension secondary to severe mitral stenosis) helps the maintenance of this flutter circuit.
Atrial flutter in mitral stenosis: Different conduction ratios are seen – 2:1, 3:1 and 4:1. Atrial rate is around 360/min, ventricular rate is varying between 90/min and 180/min.