Arrhythmias in Ebstein’s anomaly
Arrhythmias in Ebstein’s anomaly
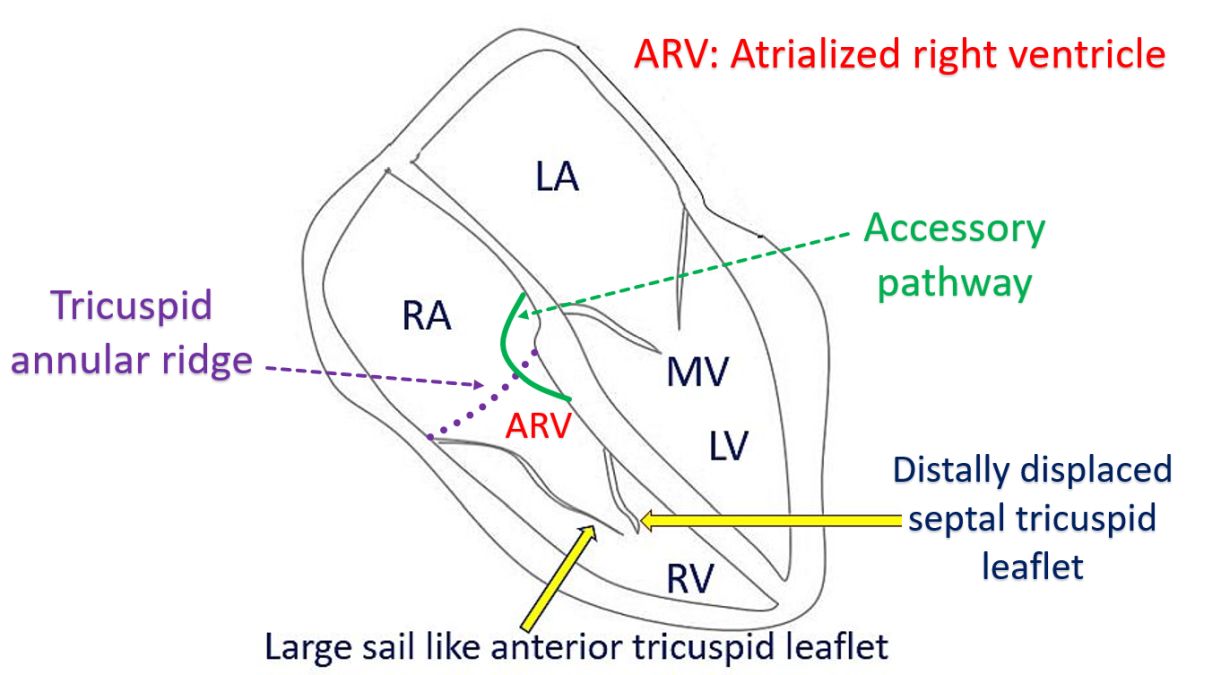
Cardiac arrhythmias are common in Ebstein’s anomaly of tricuspid valve. Accessory pathways located along the abnormal tricuspid valve is the most important cause of arrhythmias associated with Ebstein’s anomaly. Accessory pathways are muscle bundles extending from the atrial myocardium to the ventricular myocardium across the annulus fibrosus. Accessory pathways may be seen in about one third of patients with Ebstein’s anomaly. Other types of arrhythmia seen in Ebstein’s anomaly are ectopic atrial tachycardia, atrial flutter, intra atrial re-entrant tachycardia, atrial fibrillation and ventricular tachyarrhythmia.
In study of 30 patients with Ebstein’s anomaly and cardiac arrhythmia, four had undergone surgeries. Among the four patients who had undergone surgery, three had atriotomy scar related atrial re-entrant tachycardia. Among the 26 unoperated patients, one had typical AV nodal re-entry tachycardia (AVNRT). The remaining had atrioventricular re-entrant tachycardia based on 39 accessory pathways, indicating that multiple accessory pathways can occur in Ebstein’s anomaly. 27 of the accessory pathways had bidirectional conduction causing WPW syndrome, while 8 had concealed conduction. Four had Mahaim fibers. 26 of the 30 patients had 39 radiofrequency catheter ablation sessions for ablation of arrhythmogenic substrates [1].
Carpentier has classified Ebstein’s anomaly into four types. In type A, functional right ventricle is adequate and anterior tricuspid leaflet is normal. In type B, functional right ventricle is small, but anterior tricuspid leaflet is normal. In type C, functional right ventricle is very small and anterior tricuspid leaflet has restricted mobility and may cause significant obstruction of the right ventricular outflow tract. In type D, functional right ventricle is only the infundibulum and anterior tricuspid leaflet is adherent to the wall [2].
Absence of right bundle branch block (RBBB) in sinus rhythm in patients with Ebstein’s anomaly and supraventricular tachycardia, is a highly sensitive and specific indicator of the presence of an ipsilateral accessory pathway [3]. Usually RBBB pattern appears in these cases after successful radiofrequency catheter ablation [4]. Absence of RBBB pattern in ECG after catheter ablation should raise the suspicion for the presence of other accessory pathways which had been missed during ablation. Absence of RBBB is explained by the activation of the right ventricle by the accessory pathway producing narrowing of the QRS complex. In Ebstein’s anomaly, the right bundle branch is underdeveloped.
The plicated atrialized right ventricle after repair of Ebstein’s anomaly is still arrhythmogenic. Some recommend incising the tricuspid annular ridge during surgery to disconnect potential accessory pathways, especially if the pre-operative ECG has not shown an RBBB pattern. Post operative ECG may show fractionated P waves indicating areas of slow conduction and scars which can predispose to intra atrial re-entry.
While conventional accessory pathways except those in permanent junctional reciprocating tachycardia (PJRT) [5] are non responsive to adenosine, accessory pathways in Ebstein’s anomaly can respond to adenosine and verapamil [4]. In one case, the tachycardia ECG showed left bundle branch like pattern with superior axis and was terminated with injection verapamil. Detailed mapping showed an atriofascicular pathway located in the right posterolateral region, which was successfully ablated. RBBB pattern with splintered QRS characteristic of Ebstein’s anomaly was noted after ablation [4].
Sudden death in Ebstein’s anomaly is another important concern. In a study of 968 patients spanning over 4 decades, from Mayo Clinic, 0.74% had placement of an implantable cardioverter-defibrillator (ICD). Of the 968 patients in the study, 79.8% had severe Ebstein’s anomaly and 18.6% had accessory pathway. Cumulative incidence of sudden death increased as age advanced. It was 0.8% at 10 years and 14.6% at 70 years. Previous episode of ventricular tachycardia, heart failure, tricuspid valve surgery, syncope, pulmonary stenosis and hemoglobin level above 15 g/dL were the multivariable predictors of sudden death [6].
References
- Hebe J. Ebstein’s anomaly in adults. Arrhythmias: diagnosis and therapeutic approach. Thorac Cardiovasc Surg. 2000 Aug;48(4):214-9. doi: 10.1055/s-2000-6897. PMID: 11005595.
- Carpentier A, Chauvaud S, Macé L, Relland J, Mihaileanu S, Marino JP, Abry B, Guibourt P. A new reconstructive operation for Ebstein’s anomaly of the tricuspid valve. J Thorac Cardiovasc Surg. 1988 Jul;96(1):92-101. PMID: 3386297.
- Gonzalez-Melchor L, Nava S, Iturralde P, Marquez MF. The relevance of looking for right bundle branch block in catheter ablation of Ebstein’s anomaly. J Electrocardiol. 2017 Nov-Dec;50(6):894-897. doi: 10.1016/j.jelectrocard.2017.06.013. Epub 2017 Jun 17. PMID: 28666538.
- Gangurde PB, Tidake A, Shah H, Mahajan A, Lokhandwala Y, Nathani P. Absent right bundle branch block: Is it a clue of pre-excitation in Ebstein’s anomaly? Indian Heart J. 2016 Sep;68 Suppl 2(Suppl 2):S182-S185. doi: 10.1016/j.ihj.2015.11.001. Epub 2015 Dec 18. PMID: 27751284; PMCID: PMC5067457.
- Kylat RI, Samson RA. Permanent junctional reciprocating tachycardia in infants and Children. J Arrhythm. 2019 May 15;35(3):494-498. doi: 10.1002/joa3.12193. PMID: 31293698; PMCID: PMC6595346.
- Attenhofer Jost CH, Tan NY, Hassan A, Vargas ER, Hodge DO, Dearani JA, Connolly H, Asirvatham SJ, McLeod CJ. Sudden death in patients with Ebstein anomaly. Eur Heart J. 2018 Jun 1;39(21):1970-1977a. doi: 10.1093/eurheartj/ehx794. PMID: 29315367.

