Cardiac memory
Cardiac memory
Cardiac memory is the persistence of T wave changes in the ECG after normalization of a wide QRS rhythm [1]. It is a remodeling phenomenon of cardiac repolarization when there is a change in the ventricular depolarization for a period of time. It can occur after ventricular pacing, transient bundle branch block, intermittent pre-excitation, ventricular tachycardia or frequent ventricular premature beats [2].
The term cardiac memory was introduced by Rosenbaum MB et al in 1982 [3]. That seminal work showed that T wave changes may persist for days or weeks after the provoking stimulus which causes the change in activation sequence is discontinued.
Supraventricular tachycardia can also evoke cardiac memory, particularly when the ventricular activation is irregular as in atrial fibrillation (AF) [2]. Cardiac memory manifests with a change of T wave vector, usually with T wave inversion. The T wave memorizes the QRS vector of the abnormal rhythm which preconditions the myocardium. The repolarization abnormalities usually manifests after the normalization of ventricular activation [3]. It is mentioned that cardiac memory actually starts with the abnormal ventricular activation, but is masked by the secondary repolarization abnormality of the abnormal activation [2]. The persistence of the cardiac memory depends on the duration of the abnormal activation. Persistent T wave inversion for hours to days after an episode of AF with fast ventricular rate makes us presume that AF had been there for some time. Similarly, T wave changes may take a few weeks to resolve after catheter ablation of accessory pathway in a patient with pre-excitation since birth.
T wave inversions due to cardiac memory is often mistaken for T inversion due to myocardial ischemia or infarction. Most common situations leading to cardiac memory like left bundle branch block and right ventricular apical pacing have wide QRS complexes which are negative in several leads. Therefore memorizing this pattern, cardiac memory appears as T wave inversions when sinus rhythm is established later. This is how it was recognized initially [1].
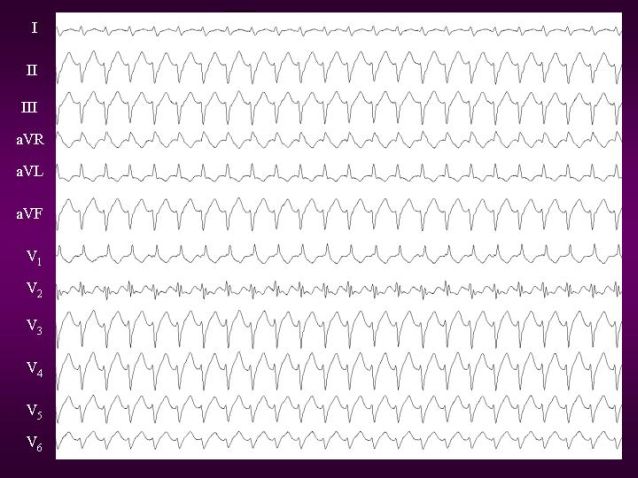
Cardiac memory has been used to localize origin of arrhythmia. For example, consider a patient presenting with palpitation and no structural heart disease, but showing inferior T wave inversion and tall peaked T waves in right precordial leads in sinus rhythm. In the absence of ischemia, this can be considered as a marker of a wide QRS rhythm originating from the inferior septal region of the left ventricle. This can be a manifestation after conversion of posterior fascicular tachycardia [1]. These cardiac memory T waves follow the typical QRS morphology of posterior fascicular tachycardia with positive QRS complexes in right precordial leads and negative QRS complexes in inferior leads (image below).
References
- Shvilkin A, Huang HD, Josephson ME. Cardiac memory: diagnostic tool in the making. Circ Arrhythm Electrophysiol. 2015 Apr;8(2):475-82.
- Siontis KC, Wen S, Asirvatham SJ. Cardiac memory for the clinical electrophysiologist. J Cardiovasc Electrophysiol. 2019 Oct;30(10):2140-2143.
- Rosenbaum MB, Blanco HH, Elizari MV, Lázzari JO, Davidenko JM. Electrotonic modulation of the T wave and cardiac memory. Am J Cardiol. 1982 Aug;50(2):213-22.
- Francis J, Venugopal K, Khadar SA, Sudhayakumar N, Gupta AK. Idiopathic Fascicular Ventricular Tachycardia. Indian Pacing Electrophysiol. J. 2004;4(3):98-103.
- Shvilkin A, Ho KK, Rosen MR, Josephson ME. T-vector direction differentiates postpacing from ischemic T-wave inversion in precordial leads. Circulation. 2005 Mar 1;111(8):969-74.


