Collection of a few ECGs in congenital heart diseases
Classical QRS pattern in ASD is the rSR’ in V1 suggestive incomplete RBBB. This pattern in ASD is due to RV volume overload. QRS axis is usually rightward, more so when there is severe PAH. Left axis deviation is feature of ostium primum ASD. First degree AV block may be noted in both primum and secundum ASD. Familial ASD with first degree AV block has been reported in secundum ASD. This type of familial ASD has an autosomal dominant inheritance pattern. There is also a higher incidence of SCD in this group.
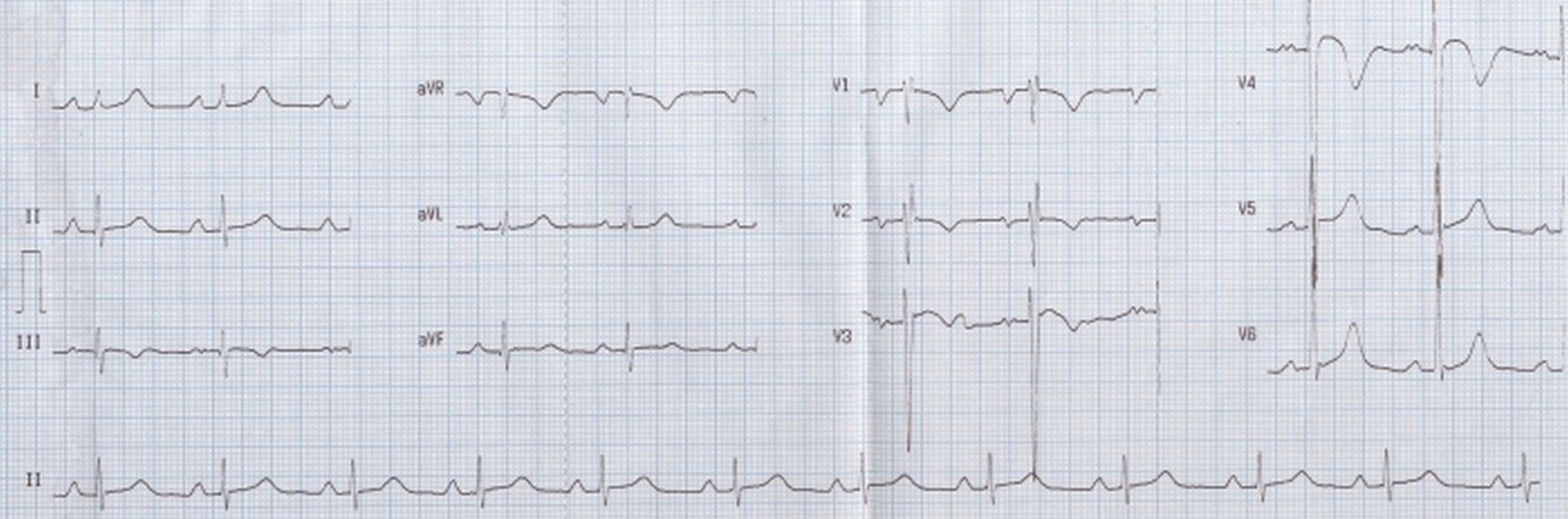
Crochetage sign in ASD, manifest as notching of R wave near the apex in inferior leads (arrows). Sharp P waves in V1 and 3 mm tall P waves in lead II suggest right atrial overload. rSr’S’ pattern in V1 is suggestive of right ventricular volume overload.
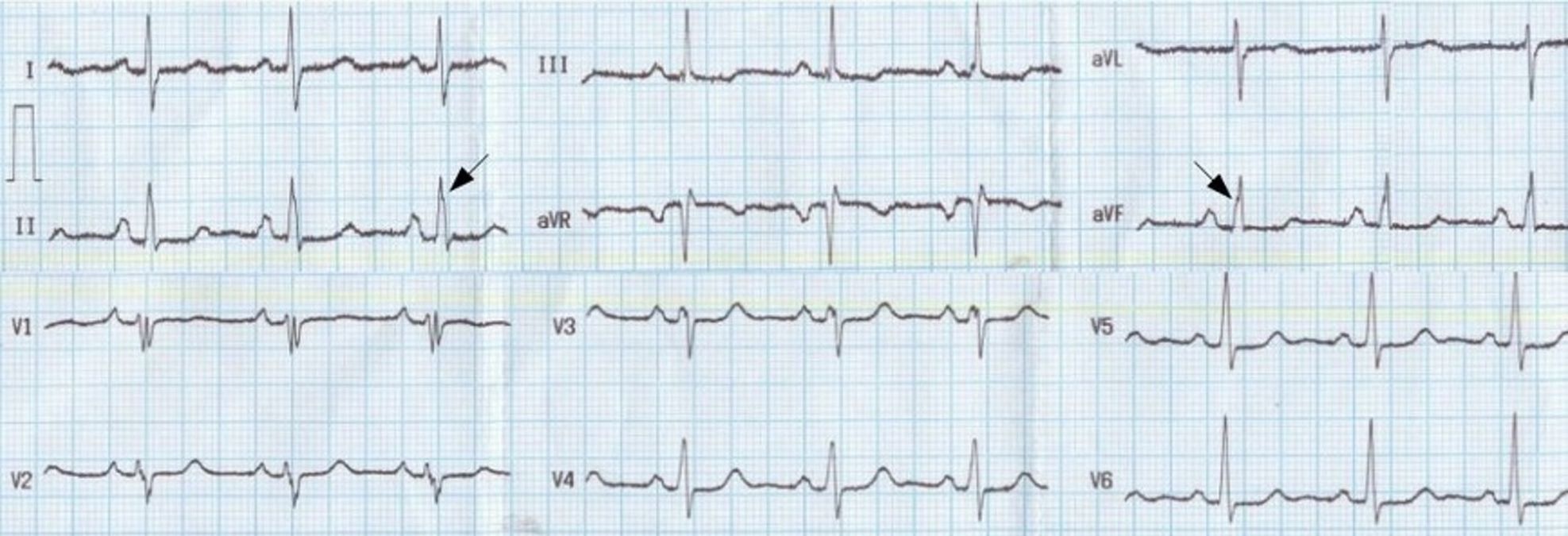
ECG in ASD with severe pulmonary hypertension: Tall R’ in V1, ST depression in inferior leads and V2-V5, and T inversion in inferior leads and V1-V6 are seen.
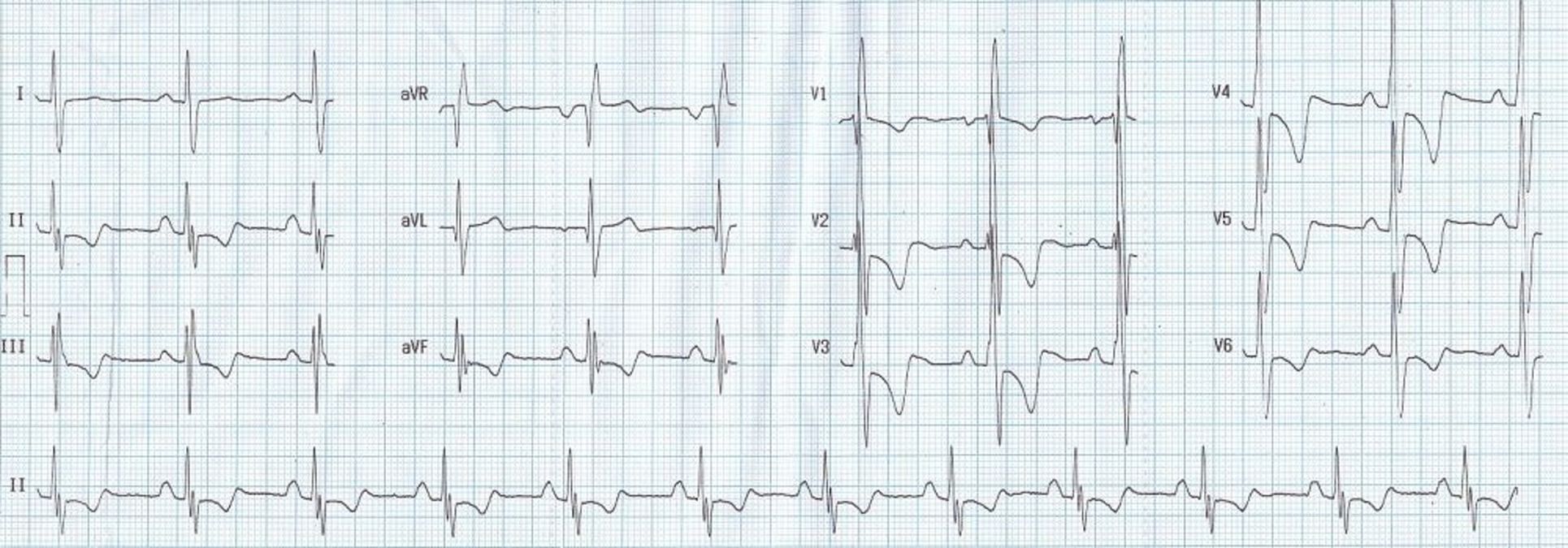
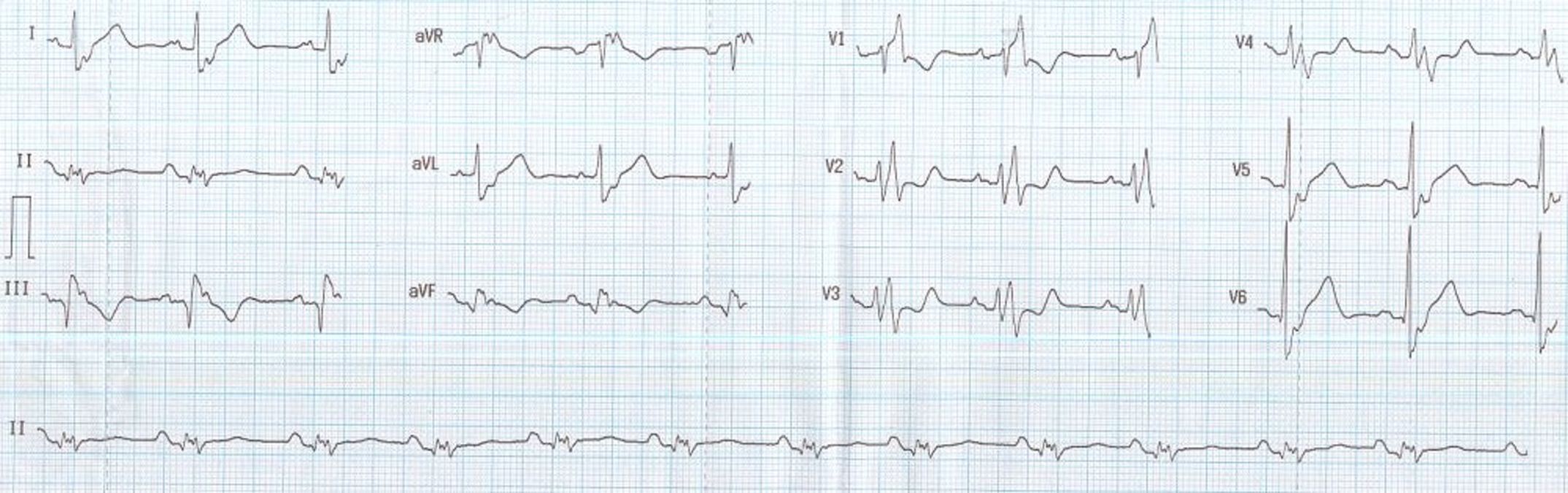
The Katz-Wachtel phenomenon/sign is tall diphasic RS complexes at least 50 mm in height in lead V2, V3 or V4 – mid precordial leads The original description by Katz and Wachtel was published in 1937. The sign has been described in VSD with biventricular hypertrophy in children. It can be seen with isolated VSD as well as complex ventricular septal defect. In fact the Circulation article cited is on Complete Transposition of the Great Vessels.
An ECG with Katz-Wachtel phenomenon is shown here. QRS amplitude is high it often overshoots the margin of the ECG graph as seen in lead V4 in this case. It may be necessary to take ECG in half standardization, that is 5 mm to a millivolt instead of 10 mm to a millivolt, to capture the full QRS complex without overlapping with other leads. Large anterior electrocardiographic forces are due to the hypertrophied right ventricle and late posterior forces due to the hypertrophied left ventricle. In addition, the ECG shows negative QRS complexes in I and aVL, indicating right axis deviation, which is a feature of right ventricular hypertrophy.
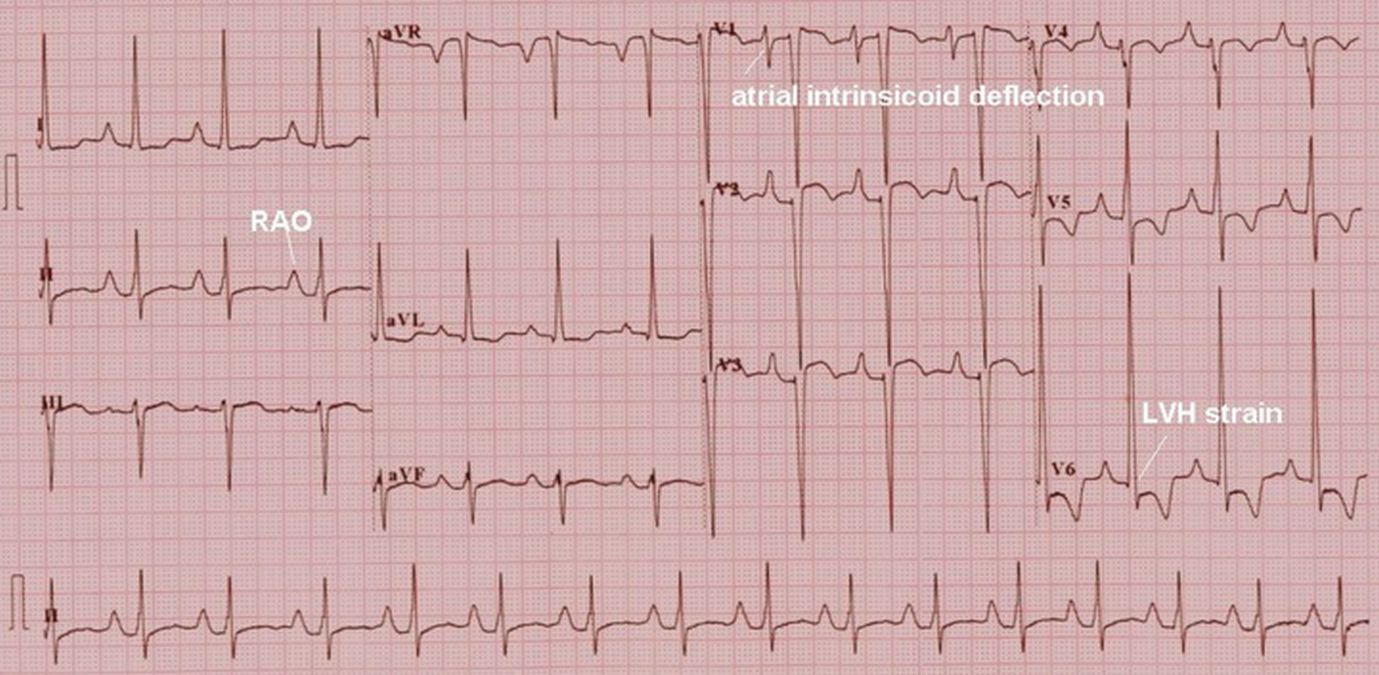
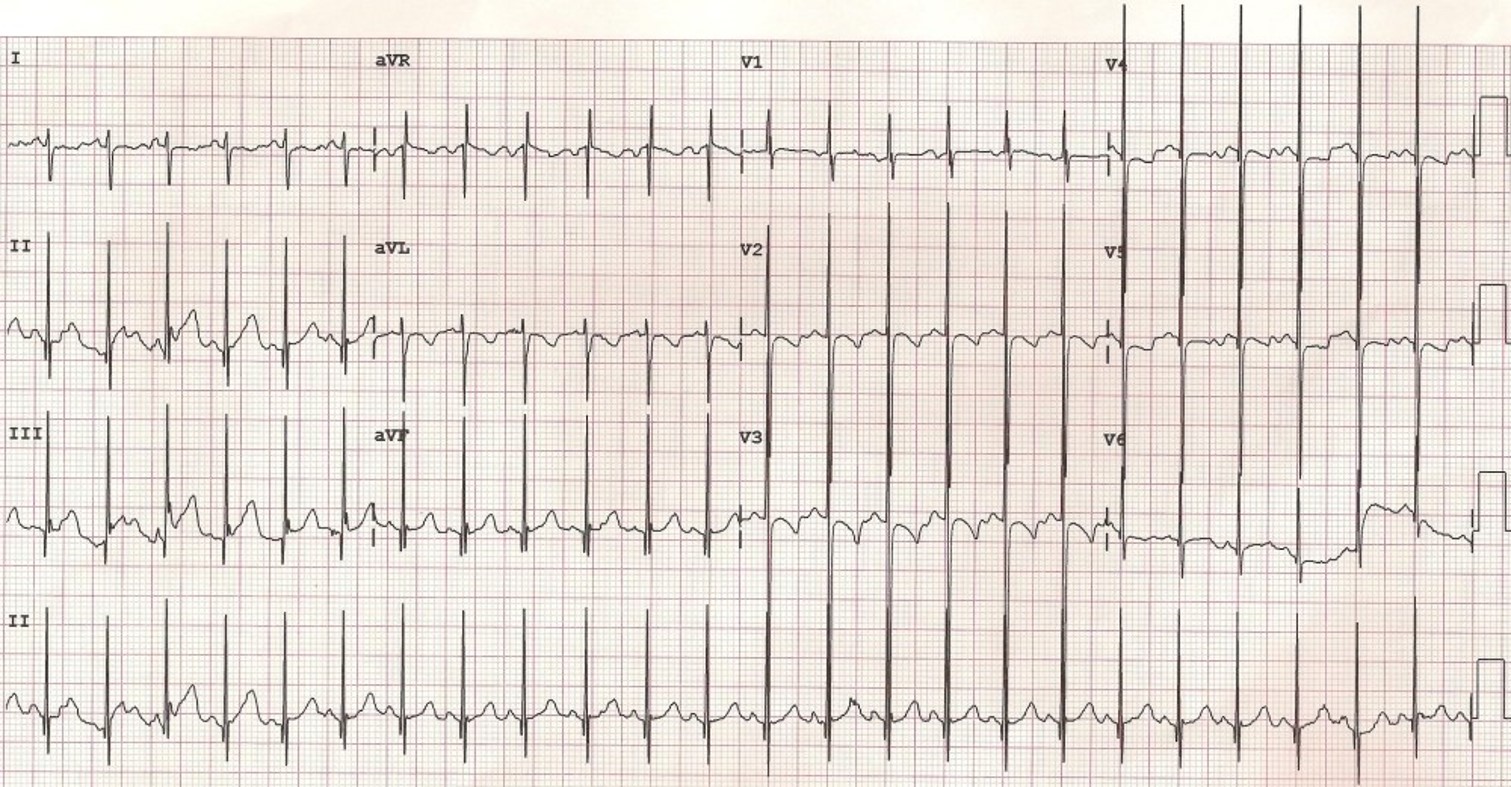
Right atrial overload is manifest as tall P waves in lead II and left ventricular hypertrophy with strain pattern is seen in lateral leads with tall R waves, ST segment depression and T wave inversion. The axis is leftward with predominantly negative QRS in leads III and aVF. The biphasic P wave in V1 with sharp atrial intrinsicoid deflection (the sharp downward deflection from the peak of the P wave to the trough of the P wave) is a pseudo left atrial overload pattern, seen in right atrial overload. In true left atrial overload the atrial intrinsicoid deflection is more slanting so that the negative component of the P wave is almost U shaped rather than the V shape in this case. All these features together in a cyanotic congenital heart disease is characteristic of tricuspid atresia.
ECG in Ebstein’s anomaly of tricuspid valve showing right bundle branch block pattern with polyphasic and splintered QRS. The QRS is wide and Lead V2 shows rsrs pattern mimicking right bundle branch block. Lead II shows multiple small deflections, that is splintered QRS. The slurred S waves in lateral leads also form part of the RBBB pattern.
The duration of QRS has been linked to right ventricular enlargement and dysfunction in Ebstein’s anomaly. A larger atrialized right ventricular volume has been noted in these cases. As a corollary, those with near normal ECG would have mild morphological abnormalities and a better clinical profile.
Splintered and polyphasic QRS of Ebstein’s anomaly can also be considered as fragmented QRS as per the new terminology. Fragmented QRS is a marker of myocardial scar and consequent arrhythmias in ischemic and nonischemic cardiomyopathy. Similarly fragmented QRS has been shown to be associated with larger region of atrialized right ventricle and increased risk of arrhythmic events in Ebstein’s anomaly.
Ebstein’s anomaly may be associated with right sided accessory pathway in ventricular pre-excitation, that is WPW syndrome, with or without atrioventricular re-entrant tachycardia. Multiple accessory pathways can occur and radiofrequency catheter ablation is effective.
Tall P waves due to gross right atrial enlargement in Ebstein’s anomaly have been called Himalayan P waves, though not seen in the ECG illustrated here. Himalayan P waves are also described in tricuspid atresia.

