Conventional CPR vs Extracorporeal CPR
Conventional CPR vs Extracorporeal CPR
Prompt initiation of cardiopulmonary resuscitation (CPR) is the key to better survival and lower morbidity after a cardiac arrest. Still survival is low even after in hospital cardiac arrest of the order of 20% while it is still lower, of the order of 10% for out of hospital cardiac arrest.
“No flow” time is the period from the onset of cardiac arrest to the initiation of chest compression. “Low flow” time is the period of conventional CPR till the achievement of ROSC (return of spontaneous circulation). Need for prolonged CPR reduces the survival. Need for CPR of 45 minutes or more has been associated with an in hospital survival of less than 2%.
It is in this setting that ECPR or extracorporeal CPR with the help of ECMO (extracorporeal membrane oxygenator) comes in for maintaining better cerebral and vital organ circulation. ECMO also gives rest to the heart allowing chance for recovery if there is a treatable cardiac cause for the cardiac arrest as by coronary revascularization. A recent study by Patricio D and associates compared ECPR vs conventional CPR [1].
Criteria for initiating ECPR in the study
Decision to initiate ECPR was base on the following criteria:
- Age less than 65 years
- Witnessed cardiac arrest
- Estimated no flow time less than 2 minutes
- Estimated ECMO placement time less than 75 minutes
- No severe comorbidity
- Signs of life during conventional CPR
Technical details of ECPR
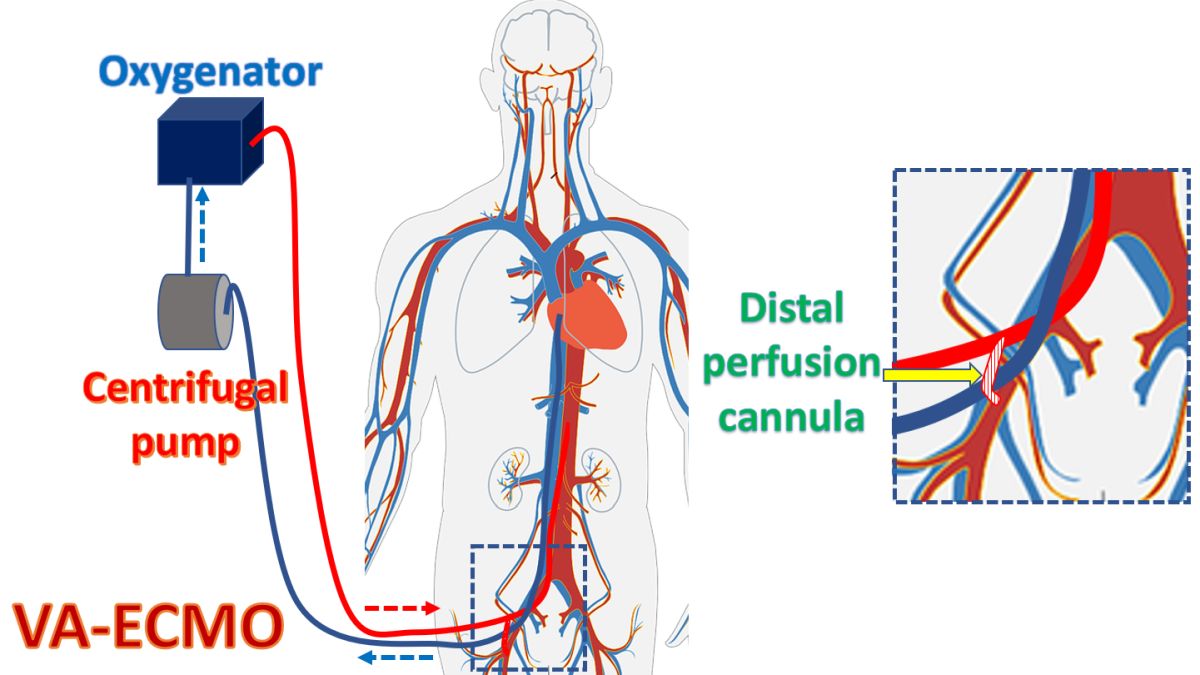
Mechanical CPR device was used if ROSC was not achieved in 3 cycles of manual CPR. ECMO was initiated by well trained ICU physicians and/or cardiac surgeons. Peripheral femoro-femoral veno-arterial ECMO with percutaneous cannulation guided by echocardiography was done under the support of mechanical CPR.
PaO2 was maintained in the range of 80-150 mm Hg, mean arterial pressure was kept above 65-70 mm Hg with vasopressors and fluids if needed and targeted temperature management aimed at a temperature of around 34 degrees centigrade for 24 hours were given. Cardiac catheterization was performed if indicated. Anticoagulation with unfractionated heparin was used. ECMO used a 25 Fr venous cannula and 18–22 Fr arterial cannula. Initial blood flow was 3-4 liters per minute and ECMO priming was with 700 ml Plasmalyte. After implantation, leg was perfused with with an anterograde single lumen 8 Fr catheter to prevent limb ischemia.
A total of 112 patients received ECPR and 523 received conventional CPR over a five year period from 2012 to 2017.
Study conclusion
The study concluded that ECPR may be associated with improved long term neurological outcome (p = 0.003).
Reference
- Patricio D, Peluso L, Brasseur A, Lheureux O, Belliato M, Vincent JL, Creteur J, Taccone FS. Comparison of extracorporeal and conventional cardiopulmonary resuscitation: a retrospective propensity score matched study. Crit Care. 2019 Jan 28;23(1):27.