Old anterior wall myocardial infarction, RBBB, LAHB
Old anterior wall myocardial infarction, RBBB, LAHB
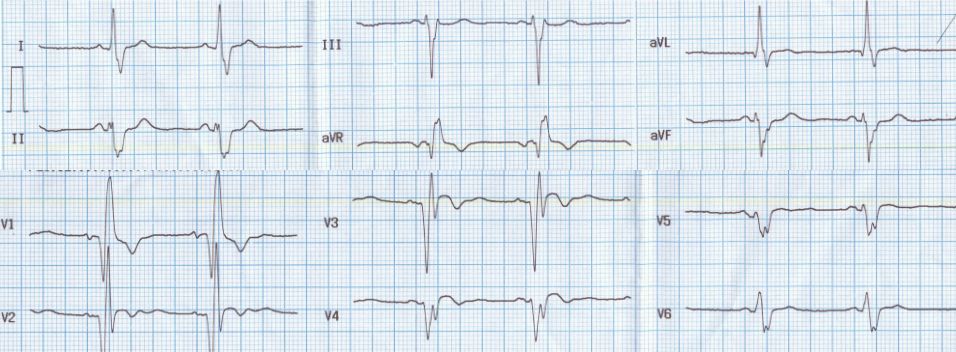
Slurred S waves in leads I, aVl and V5, V6 are suggestive of right bundle branch block. The terminal slurred R wave in V1 is also in favour of RBBB. Instead of the rSR’ pattern, there is QR pattern in V1. The QR pattern in V1 is because the initial r wave has been knocked off by anterior wall myocardial infarction. This pattern is also called a QRBBB. There are Q waves in V1 to V4, suggestive of old anterior wall myocardial infarction. Inverted T waves in V1 to V3 can be accounted for by RBBB as well as old myocardial infarction. But the ST segment is elevated, indicating the contribution of myocardial infarction, possibly with a dyskinetic segment.
There is left axis deviation of QRS, with rS pattern in leads II, III and aVF, suggestive of left anterior hemiblock. Left anterior hemiblock is also known as left anterior fascicular block. The PR interval is normal. The combination of left anterior hemiblock with right bundle branch block is called bifascicular block. This combination is the commoner form of bifascicular block, while the occurrence of left posterior hemiblock along with right bundle branch block is the rarer variety. Left posterior hemiblock is rarer because it is a larger bundle with dual blood supply, unlike the anterior fascicle and hence is likely to be damaged only in more extensive myocardial infarction. Left posterior hemiblock is characterised by right axis deviation of QRS and rS pattern in leads I and aVl. If the PR interval is prolonged in a case of bifascicular block, it will be called as trifascicular block.
QRS width of 160 ms possibly indicates more of myocardial involvement affecting the conduction system. Higher QRS width is more common with left bundle branch block than RBBB.


