Importance of lead aVR
Importance of lead aVR
Lead aVR was often ignored as all the waves are inverted in aVR in contrast to other leads. Lead aVR is thought to point to the cavity of the heart. It has been called the neglected lead [1] and the forgotten lead [2].
Lead aVR came into limelight with the identification of the significance of ST elevation in the lead indicating left main coronary artery disease. Classical electrocardiographic pattern in left main coronary artery disease is ST segment elevation in aVR with extensive ST depression in other leads, most prominent in I, II and V4-V6 [3]. ST elevation in aVR can also occur in proximal left anterior descending coronary artery disease. ST segment elevation in aVR greater than or equal to that in V1 distinguished left main stenosis from left anterior descending coronary artery (LAD) stenosis with 81% sensitivity, 80% specificity. ST segment elevation in aVR in proximal LAD occlusion before first septal is thought to be due to transmural ischemia of the basal part of the septum [4]. Injury current of basal part of septum is directed towards right shoulder and aVR. ST segment elevation in aVR noted in left main disease is also likely due to the same mechanism as flow to first septal is blocked in this case as well. Mortality was more frequently observed in left main obstruction patients with higher degree of ST elevation in aVR [5].
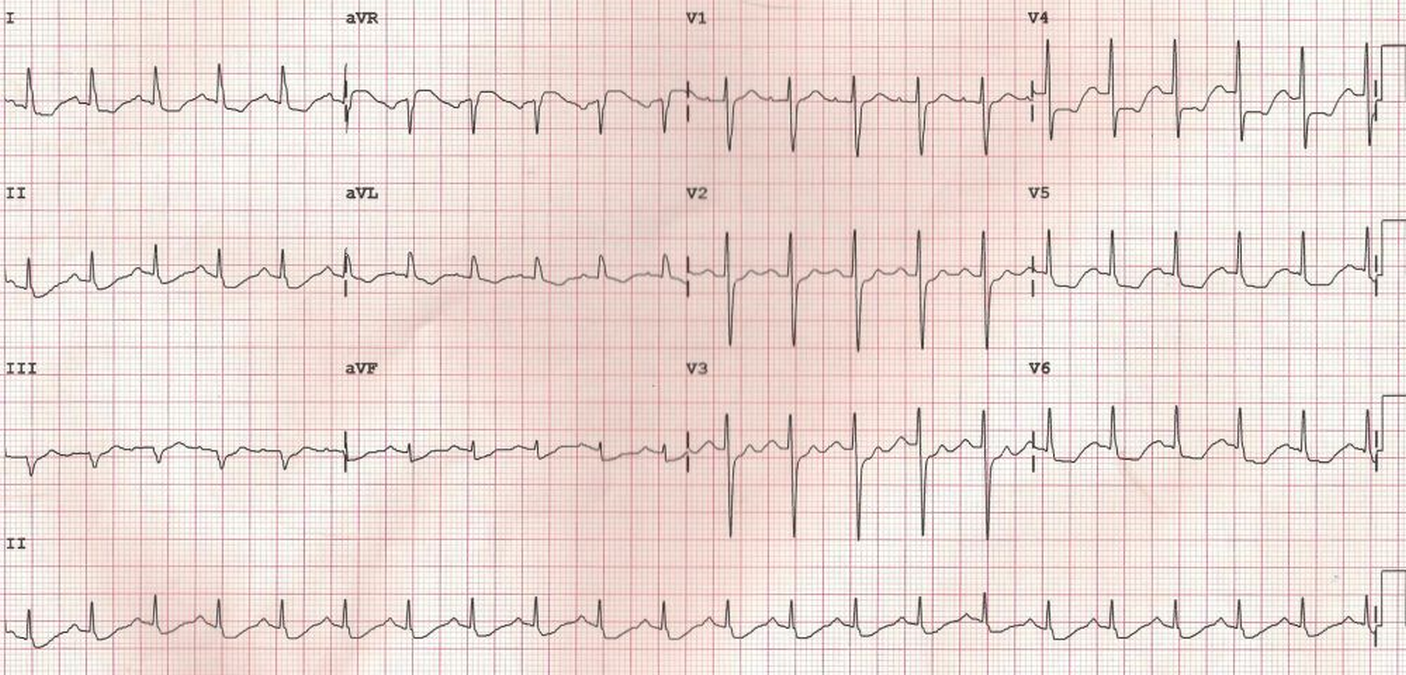
ECG in a person with persistent anginal pain for the past several hours showing significant ST segment depression in anterolateral leads along with sinus tachycardia. ST segment elevation is noted in aVR. Such a pattern is consistent with significant left main coronary artery stenosis.
Tall R wave in aVR has been called as the Goldberger’s sign in left ventricular aneurysm [6]. Usual ECG finding in left ventricular aneurysm is persistent ST segment elevation.
In acute pericarditis, when ST segment elevation is noted in all other leads, ST segment depression is seen in aVR [7]. Similarly, while PR segment is depressed in other leads in acute pericarditis, it is elevated in aVR. Lead V1 may also show changes similar to aVR in acute pericarditis as it is also a cavity oriented lead like aVR.
ST segment depression in aVR on admission has been shown to predict larger infarct and left ventricular dysfunction despite successful reperfusion in anterolateral myocardial infarction [8].
aVR sign has been described in Brugada syndrome. A prominent R wave in lead aVR (aVR sign in Brugada syndrome) has been suggested as marker for development of life threatening arrhythmic events in Brugada syndrome by Babai Bigi MA and associates [9]. They proposed that a prominent final R wave in lead aVR may indicate more right ventricular conduction delay and hence more electrical heterogeneity, which can cause a higher risk of arrhythmia. R wave amplitude of 0.3 mV or more OR R/q 0.75 or more have been considered as significant. Over three fourths of recurrent arrhythmic events were in those with aVR sign. More than eighty percent of Brugada syndrome patients with the sign in their study had arrhythmic events on follow up. At the same time only about a quarter of those without aVR sign had arrhythmic events on follow up. R’/S ratio in aVR (aVR sign) has been associated with AA genotype carriers compared to G allele carriers in Brugada syndrome with SCN5A mutations [10].
References
- Chenniappan M, Sankar RU, Saravanan K, Karthikeyan. Lead aVR–the neglected lead. J Assoc Physicians India. 2013 Sep;61(9):650-4.
- Ching S, Ting SM. The Forgotten Lead: aVR in Left Main Disease. Am J Med. 2015 Dec;128(12):e11-3.
- Sen F, Ozeke O, Kirbas O, Burak C, Kafes H, Tekin Tak B, Ozdamar U, Ocak K, Topaloglu S, Aras D. Classical electrocardiographic clues for left main coronary artery disease. Indian Heart J. 2016 Sep;68 Suppl 2(Suppl 2):S226-S227.
- Engelen DJ, Gorgels AP, Cheriex EC, De Muinck ED, Ophuis AJ, Dassen WR, Vainer J, van Ommen VG, Wellens HJ. Value of the electrocardiogram in localizing the occlusion site in the left anterior descending coronary artery in acute anterior myocardial infarction. J Am Coll Cardiol. 1999 Aug;34(2):389-95.
- Yamaji H, Iwasaki K, Kusachi S, Murakami T, Hirami R, Hamamoto H, Hina K, Kita T, Sakakibara N, Tsuji T. Prediction of acute left main coronary artery obstruction by 12-lead electrocardiography. ST segment elevation in lead aVR with less ST segment elevation in lead V(1). J Am Coll Cardiol. 2001 Nov 1;38(5):1348-54.
- Ola O, Dumancas C, Mene-Afejuku TO, Akinlonu A, Al-Juboori M, Visco F, Mushiyev S, Pekler G. Left Ventricular Aneurysm May Not Manifest as Persistent ST Elevation on Electrocardiogram. Am J Case Rep. 2017 Apr 16;18:410-413.
- Spodick DH. Diagnostic electrocardiographic sequences in acute pericarditis. Significance of PR segment and PR vector changes. Circulation. 1973 Sep;48(3):575-80.
- Kosuge M, Kimura K, Ishikawa T, Endo T, Hongo Y, Shigemasa T, Iwasawa Y, Tochikubo O, Umemura S. ST-segment depression in lead aVR predicts predischarge left ventricular dysfunction in patients with reperfused anterior acute myocardial infarction with anterolateral ST-segment elevation. Am Heart J. 2001 Jul;142(1):51-7.
-
Babai Bigi MA, Aslani A, Shahrzad S. aVR sign as a risk factor for life-threatening arrhythmic events in patients with Brugada syndrome. Heart Rhythm. 2007 Aug;4(8):1009-12.
- Lizotte E, Junttila MJ, Dube MP, Hong K, Benito B, DE Zutter M, Henkens S, Sarkozy A, Huikuri HV, Towbin J, Vatta M, Brugada P, Brugada J, Brugada R. Genetic modulation of brugada syndrome by a common polymorphism. J Cardiovasc Electrophysiol. 2009 Oct;20(10):1137-41.