Limitations of pulse oximetry
Limitations of pulse oximetry
Pulse oximeter is a handy tool at the beside to get an immediate assessment of the oxygen saturation of arterial blood. Still, it has several limitations and arterial blood gas analysis (ABG) is the gold standard for assessment of arterial oxygen saturation. But ABG is more cumbersome, requires an arterial puncture, which is not easy always and the results are not available immediately. So pulse oximetry is often used as a surrogate for ABG at the beside for taking immediate decisions.
Poor signal is one of the important limitations in many situations. Poor signal can occur due to vasoconstriction in a cold limb and in shock. Warming the fingers is often useful in case of a cold limb. Cardiac arrest and respiratory arrest are other reasons for poor signals. Edema, cardiac arrhythmia and arteriovenous fistula can also affect the quality of pulse oximetry signals. Blue, green and black nail polish has been shown to affect the signal in studies.
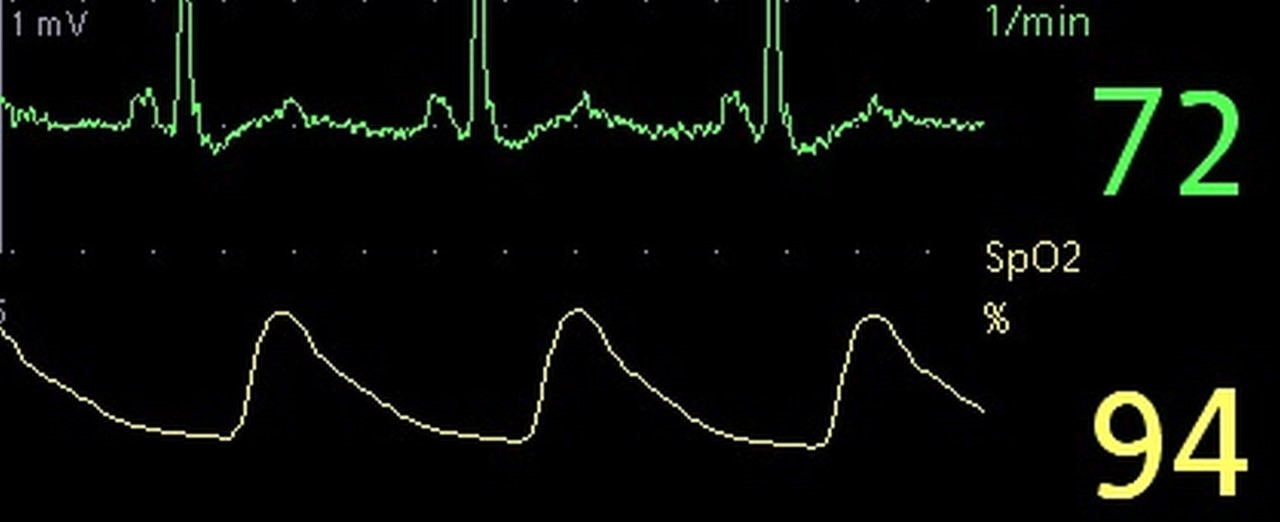
Another situation which can temporarily affect the signal is automatic inflation of a non-invasive blood pressure cuff. But this recovers soon after deflation of the cuff. A sensor which is contaminated with dirt can also cause poor signal. Movement of the finger, tremors and elevation of the finger above the level of the heart can also cause poor signals. A poor signal can be recognized by a bad plethysmography tracing and steps can be taken to rectify it.
It is mentioned that bright light falling on the sensor, either natural or artificial, can cause an increase in the signal and give a falsely higher value of pulse oximetry. In the hospital setting, the simple method is to switch off a bright light source if present and recheck. Of course, this is not applicable in case of bright sunlight! Carbon monoxide poisoning can give a falsely high reading of 100% [1]. It may be noted that false elevation may be noted soon after smoking, due to the carbon monoxide in smoke.
A prospective study reported 25 pulse oximetry measurements with concurrent ABG in 16 adults with carbon monoxide exposure. Oxygen saturation measured by pulse oximetry failed to decrease to less than 96% despite carboxyhemoglobin levels as high as 44%. Pulse oximetry was found to overestimate oxyhemoglobin saturation by the amount of carboxyhemoglobin present. Authors concluded that pulse oximetry is unreliable in estimating oxyhemoglobin saturation in carbon monoxide exposed patients and should be interpreted with caution in smokers [2].
Pulse oximeter overestimated oxygen saturation by an amount proportional to the concentration of methemoglobin in one study [3]. Another report also mentioned that pulse oximeter overestimates oxygen saturation in methemoglobinemia [4]. Pulse CO-oximeters are special devices which can additionally monitor non-invasively the fractional carboxyhemoglobin and methemoglobin content in blood. A study in healthy adults has shown that methemoglobin readings can become progressively more inaccurate as arterial oxygen saturation decreases below 95%. At times it can overestimate true values of methemoglobin by 10% to 40%. But in this study, methemoglobin caused pulse oximetry to underestimate arterial oxygen saturation at high saturation [5].
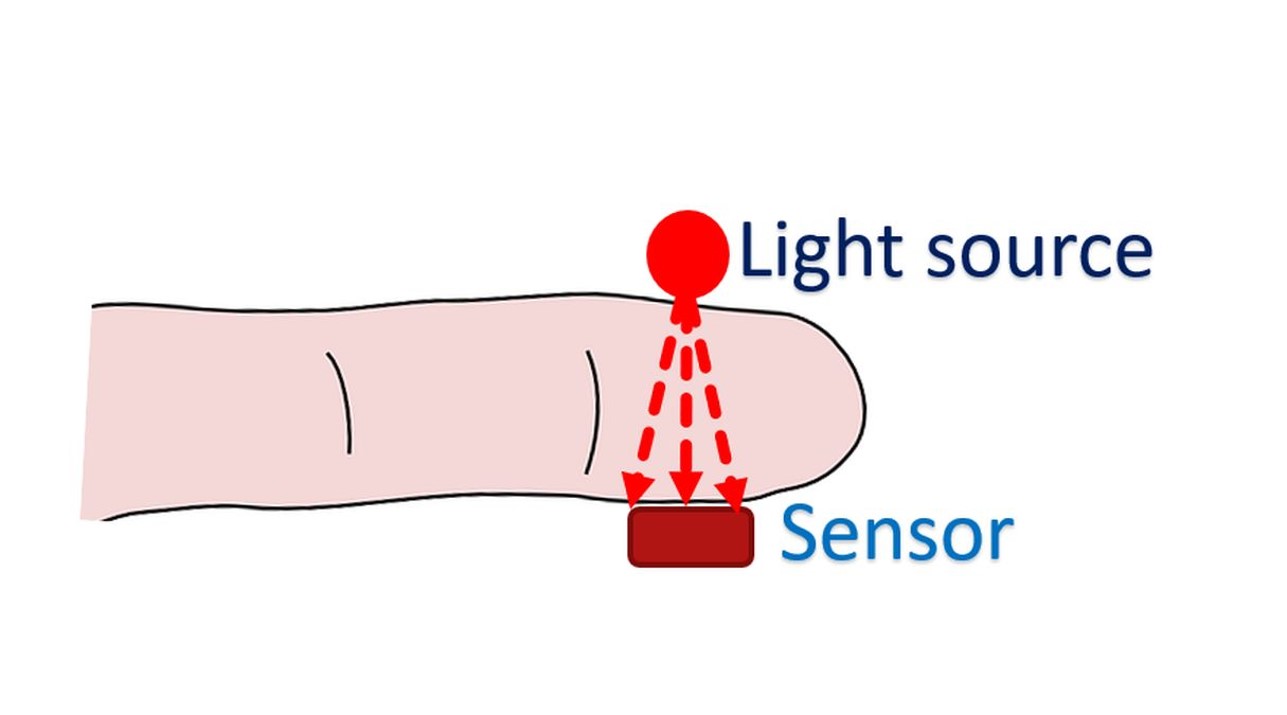
Laboratory equipment uses multiwavelength oximeter and can measure precisely and simultaneously, the concentrations of oxyhemoglobin, deoxyhemoglobin, methemoglobin and carboxyhemoglobin. Pulse oximeter LED emits two wavelengths of light, usually at 660 nm and 925 nm for measuring saturations of oxyhemoglobin and deoxyhemoglobin. If the optical spectra of diagnostically used dyes in blood overlap with those of oxyhemoglobin or deoxyhemoglobin, it can interfere with the accuracy of pulse oximetry readings.
Methylene blue, indigo carmine and indocyanine green were studied in volunteers in a study. Of the three, indigo carmine produced the least changes in pulse oximetry readings. Methylene blue had the highest absorbance at 660 nm and that explained the highest degree of interference in measurement of oxygen saturation by pulse oximeter [6].
In cyanide poisoning, normal oxygen saturation is expected on pulse oximetry as there is adequate oxygen in blood, but there is inability to use the oxygen at the tissue level. It follows that venous blood gas analysis will show high partial pressure of oxygen and high oxygen saturation. Cyanide poisoning is an example of cytotoxic anoxia caused by inhibition of cytochrome oxidase preventing utilization of oxygen by tissues. Excessively rapid infusion of sodium nitroprusside can cause features of cyanide toxicity as it can be metabolized to cyanide and later detoxified to thiocyanate.
There are some reports that pulse oximetry is inaccurate with hemoglobin levels below 5 gm/dL. One study evaluated 17 nonhypoxic patients with initial hematocrit of less than 20% due to gastrointestinal bleeding or blunt trauma. They noted that difference between pulse oximetry and arterial blood gas analysis values of oxygen saturation was not statistically significant in a hemoglobin range from 2.3 to 8.7 g/dL [7].
Pulse oximeters are usually calibrated with studies in adults. It may be felt that fetal hemoglobin in infants may alter the values. One study evaluated 22 preterm infants varying from one hour to 73 days of age. They concluded that pulse oximeter gives reliable oxygen saturation measurements, unaffected by the fetal hemoglobin level in preterm infants [8]. But in a systematic review, five studies showed that an increase in fetal hemoglobin changes the relation of partial pressure of oxygen to oxygen saturation measured by pulse oximetry. The physiological explanation was the leftward shift in oxygen dissociation curve [9].
Pulse oximetry may give variable results in sickle cell disease. Patients with sickle cell disease usually have mild hypoxemia. Their oxygen dissociation curve is shifted to the right. This would mean that oxygen saturation in sickle cell disease should be lower than normal [10]. Another outpatient study of 21 children with sickle cell disease also concluded that making treatment decisions based on pulse oximetry alone in those who are not acutely ill may be inappropriate [11].
References
- Susan DeMeulenaere S. Pulse Oximetry: Uses and Limitations. 2007; 3(5):312-317. DOI:https://doi.org/10.1016/j.nurpra.2007.02.021
- Buckley RG, Aks SE, Eshom JL, Rydman R, Schaider J, Shayne P. The pulse oximetry gap in carbon monoxide intoxication. Ann Emerg Med. 1994 Aug;24(2):252-5. doi: 10.1016/s0196-0644(94)70137-7. PMID: 8037391.
- Barker SJ, Tremper KK, Hyatt J. Effects of methemoglobinemia on pulse oximetry and mixed venous oximetry. Anesthesiology. 1989 Jan;70(1):112-7. doi: 10.1097/00000542-198901000-00021. PMID: 2912291.
- Watcha MF, Connor MT, Hing AV. Pulse oximetry in methemoglobinemia. Am J Dis Child. 1989 Jul;143(7):845-7. doi: 10.1001/archpedi.1989.02150190095030. PMID: 2741859.
- Feiner JR, Bickler PE, Mannheimer PD. Accuracy of methemoglobin detection by pulse CO-oximetry during hypoxia. Anesth Analg. 2010 Jul;111(1):143-8. doi: 10.1213/ANE.0b013e3181c91bb6. Epub 2009 Dec 10. PMID: 20007731.
- Scheller MS, Unger RJ, Kelner MJ. Effects of intravenously administered dyes on pulse oximetry readings. Anesthesiology. 1986 Nov;65(5):550-2. doi: 10.1097/00000542-198611000-00023. PMID: 3777490.
- Jay GD, Hughes L, Renzi FP. Pulse oximetry is accurate in acute anemia from hemorrhage. Ann Emerg Med. 1994 Jul;24(1):32-5. doi: 10.1016/s0196-0644(94)70158-x. PMID: 8010546.
- Rajadurai VS, Walker AM, Yu VY, Oates A. Effect of fetal haemoglobin on the accuracy of pulse oximetry in preterm infants. J Paediatr Child Health. 1992 Feb;28(1):43-6. doi: 10.1111/j.1440-1754.1992.tb02615.x. PMID: 1372809.
- Pritišanac E, Urlesberger B, Schwaberger B, Pichler G. Accuracy of Pulse Oximetry in the Presence of Fetal Hemoglobin-A Systematic Review. Children (Basel). 2021 Apr 30;8(5):361. doi: 10.3390/children8050361. PMID: 33946236; PMCID: PMC8145233.
- Pianosi P, Charge TD, Esseltine DW, Coates AL. Pulse oximetry in sickle cell disease. Arch Dis Child. 1993 Jun;68(6):735-8. doi: 10.1136/adc.68.6.735. PMID: 8333761; PMCID: PMC1029363.
- Blaisdell CJ, Goodman S, Clark K, Casella JF, Loughlin GM. Pulse oximetry is a poor predictor of hypoxemia in stable children with sickle cell disease. Arch Pediatr Adolesc Med. 2000 Sep;154(9):900-3. doi: 10.1001/archpedi.154.9.900. PMID: 10980793.