Localisation of Ventricular Tachycardia by Surface ECG
Localisation of Ventricular Tachycardia by Surface ECG
Surface ECG can be used to identify the site of origin of ventricular tachycardia. QRS morphologic patterns and vectors are helpful in discerning the activation pattern of the myocardium. Chest wall deformity as well as metabolic and drug effects can cause limitations in analysis sometimes [1]. Identification of site of origin of VT is useful while planning catheter ablation. It is also useful in correlating with the clinical situation as in post myocardial infarction scar related VT. Another instance is for correlation with findings on imaging modalities like echocardiography and cardiac magnetic resonance imaging [2].
Fascicular VT is one type, the site of origin of which is familiar to most of us. Original description dates back to Belhassen et al in 1981 [3]. Left posterior fascicular VT has a right bundle branch block pattern with left superior axis and RS complexes in V5, V6. Scar VT after inferior wall myocardial infarction can resemble fascicular VT, though the QRS will be wider.
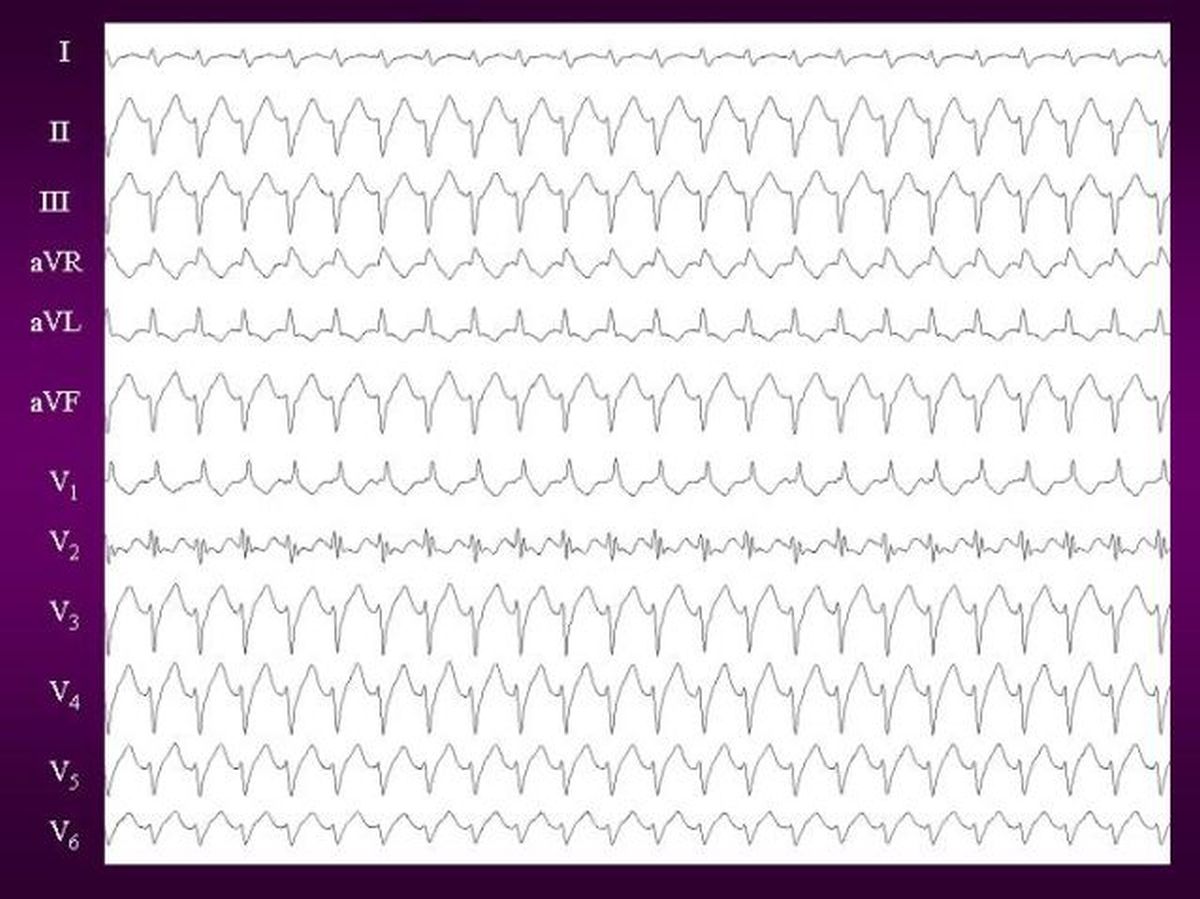
Epicardial origin of ventricular tachycardia can occur in about 15% of cases. It is important to identify these pre-procedure, as an epicardial approach for mapping and ablation will be needed. ECG features suggesting epicardial origin of VT has been discussed earlier and include interval criteria and morphology criteria [5,6].
Interval criteria are:
- Intrinsicoid deflection time ≥ 85 msec
- Shortest RS complex ≥121 ms
- Maximum deflection index ≥0.55
Morphology criteria are:
- Q waves in lead I and no q waves in inferior leads
- Pseudo delta wave ≥34 ms
Outflow tract VT is the commonest variety in those without structural heart disease. In general they have inferior axis with positive QRS complexes in II, III and aVF. Close anatomical relationship of posteroseptal RVOT with LVOT, distal coronary sinus and coronary arteries make differentiation from surface ECG challenging, though important while planning ablation.
Ventricular arrhythmias originating from the aortic root are also known as aortic cusp VTs. R wave in lead aVL is said to rule out origin in the left coronary cusp, right coronary cusp or the junction between the two. VT arising from left coronary cusp has RBBB pattern with inferior axis [2]. Of course, this pattern would overlap with that of some fascicular VTs.
Papillary muscle VT originating from left anterolateral papillary muscle will have RBBB pattern with right inferior axis while that from left inferoseptal papillary muscle will have RBBB pattern with right or left superior axis [2]. Again, these patterns are similar to those of fascicular VTs. To complicate matters further, mitral annular VT can also have RBBB pattern! VT can also originate from the tricuspid annulus, with LBBB pattern as well as from right ventricular papillary muscles.
References
- Park KM, Kim YH, Marchlinski FE. Using the surface electrocardiogram to localize the origin of idiopathic ventricular tachycardia. Pacing Clin Electrophysiol. 2012 Dec;35(12):1516-27. doi: 10.1111/j.1540-8159.2012.03488.x. Epub 2012 Aug 16. PMID: 22897344.
- Condori Leandro HI, Lebedev DS, Mikhaylov EN. Discrimination of ventricular tachycardia and localization of its exit site using surface electrocardiography. J Geriatr Cardiol. 2019 Apr;16(4):362-377. doi: 10.11909/j.issn.1671-5411.2019.04.008. PMID: 31105757; PMCID: PMC6503474.
- Belhassen B, Rotmensch HH, Laniado S. Response of recurrent sustained ventricular tachycardia to verapamil. Br Heart J. 1981 Dec;46(6):679-82. doi: 10.1136/hrt.46.6.679. PMID: 7317238; PMCID: PMC482717.
-
Francis J, Venugopal K, Khadar SA, Sudhayakumar N, Gupta AK. Idiopathic fascicular ventricular tachycardia. Indian Pacing Electrophysiol J. 2004 Jul 1;4(3):98-103. PMID: 16943977; PMCID: PMC1501077.
-
Vallès E, Bazan V, Marchlinski FE. ECG criteria to identify epicardial ventricular tachycardia in nonischemic cardiomyopathy. Circ Arrhythm Electrophysiol. 2010 Feb;3(1):63-71. doi: 10.1161/CIRCEP.109.859942. Epub 2009 Dec 11. PMID: 20008307.
-
Berruezo A, Mont L, Nava S, Chueca E, Bartholomay E, Brugada J. Electrocardiographic recognition of the epicardial origin of ventricular tachycardias. Circulation. 2004 Apr 20;109(15):1842-7. doi: 10.1161/01.CIR.0000125525.04081.4B. Epub 2004 Apr 12. PMID: 15078793.

