Rheumatic heart disease, mitral regurgitation
Rheumatic heart disease, mitral regurgitation
Though most of the manifestations of acute rheumatic fever does not leave long lasting sequelae, carditis is different. Carditis can resolve without sequelae in a few cases, but most often it leads to valvular lesions which are progressive. The most commonly involved valve is the mitral valve and mitral regurgitation is the commonest lesion in acute rheumatic fever. Stenotic lesions do not occur in the acute phase as they take a long time to develop by progressive fibrosis. According to Paul Wood, the frequency of involvement of the valves in rheumatic fever is according to the hemodynamic load on the valve. In this respect mitral valve has the maximum load followed by aortic, tricuspid and pulmonary in that order.
Rheumatic mitral regurgitation
Rheumatic mitral regurgitation manifests clinically with a pansystolic murmur at the apex, radiating to the axilla and back. It is often associated with a left ventricular third heart sound. The radiation pattern of the murmur is due to the posterior direction of the mitral regurgitation jet as the predominant involvement is that of anterior mitral leaflet. Mitral leaflets are thickened and the closure is incomplete, leaving a regurgitant orifice. The size of the regurgitant orifice increases as the severity increases.
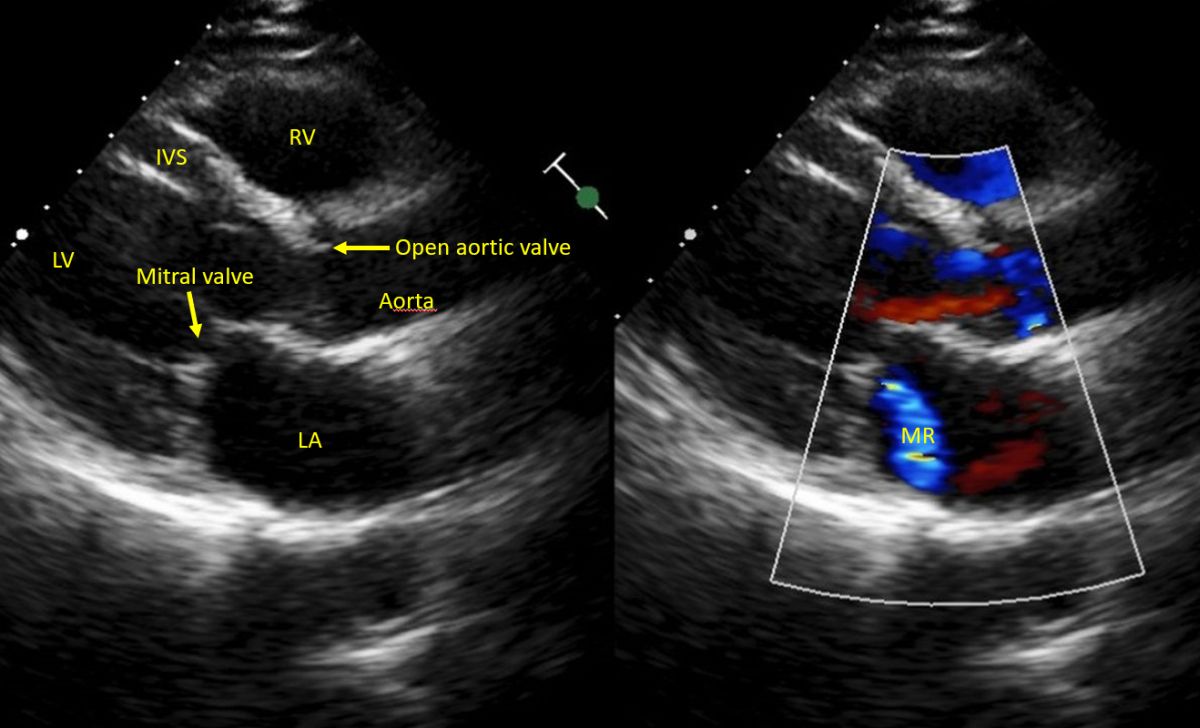
Posteriorly directed mitral regurgitation jet (MR) in bluish mosaic color, extending from the closed mitral valve to the posterior wall of left atrium. LA: Left atrium, LV: Left ventricle, IVS: Interventricular septum, RV: Right ventricle. This is a left parasternal view with the echo beam coming from the top of the image. So posterior structures will be at the lower part of the image. In color Doppler echocardiography, flow directed away from the echo transducer will be color coded blue.
Chronic mitral regurgitation can progress over the years. Mitral regurgitation produces dilatation of the left atrium and left ventricle due to the volume overload. Left ventricular dilatation enlarges the mitral valve annulus, preventing the proper coaptation of the mitral leaflets. This causes worsening of mitral regurgitation. This is often called ‘MR begets MR’. Severe mitral regurgitation produces a forceful left ventricular apex with cardiomegaly.
Acute mitral regurgitation in the setting of acute rheumatic fever can regress as the rheumatic fever subsides. It may disappear completely or persist partially as chronic rheumatic mitral regurgitation.
Chronic mitral regurgitation is often asymptomatic until the left ventricle starts to fail due to progressive dilatation and fibrosis. Since it is a volume overload lesion, palpitation may be the initial symptom, followed by exertional dyspnea and other features of heart failure later. Onset of symptoms is late in mitral regurgitation as the left ventricle has two outlets in this condition – left atrium and left ventricle. For the same reason, by the time severe symptoms occur, there may be irreversible fibrosis in the left ventricle. Such cases may not improve even after surgical treatment.
Severe symptomatic mitral regurgitation not responding to medical management can be repaired surgically or replaced with a prosthetic valve. Recently catheter based, non-surgical repair using specially designed clips to reduce the regurgitation have been innovated.