Adenosine for differentiating AVNRT from AVRT
Adenosine for differentiating AVNRT from AVRT
Adenosine is used to terminate atrioventricular node dependent arrhythmias like AV nodal reentrant tachycardia (AVNRT) and atrioventricular reentrant tachycardia (AVRT). It is also useful in the treatment of other forms of tachycardias sometimes. Use of adenosine in tachycardias could be for diagnosis of the mechanism as well. Adenosine can induce a PR jump on surface ECG in those with AVNRT which can be used to differentiate AVNRT from AVRT with concealed accessory pathway [1]. In those with concealed accessory pathway, pre-excitation will not be manifest in ECG as there is no antegrade conduction in that pathway in sinus rhythm. It takes part in the retrograde limb of reentry in AVRT [2].
Sometimes pre-excitation is not evident in the ECG because of relative competing conduction velocities between AV nodal pathway and accessory pathway. Similarly, it may not be manifest because the accessory pathway is far away from the sinus node as in left lateral pathway [3]. When adenosine prolongs the AV nodal conduction, conduction through the slower accessory pathway becomes manifest as pre-excitation. Adenosine usually has no effect on accessory pathways except for atriofascicular pathways and permanent junctional reciprocating tachycardia (PJRT).
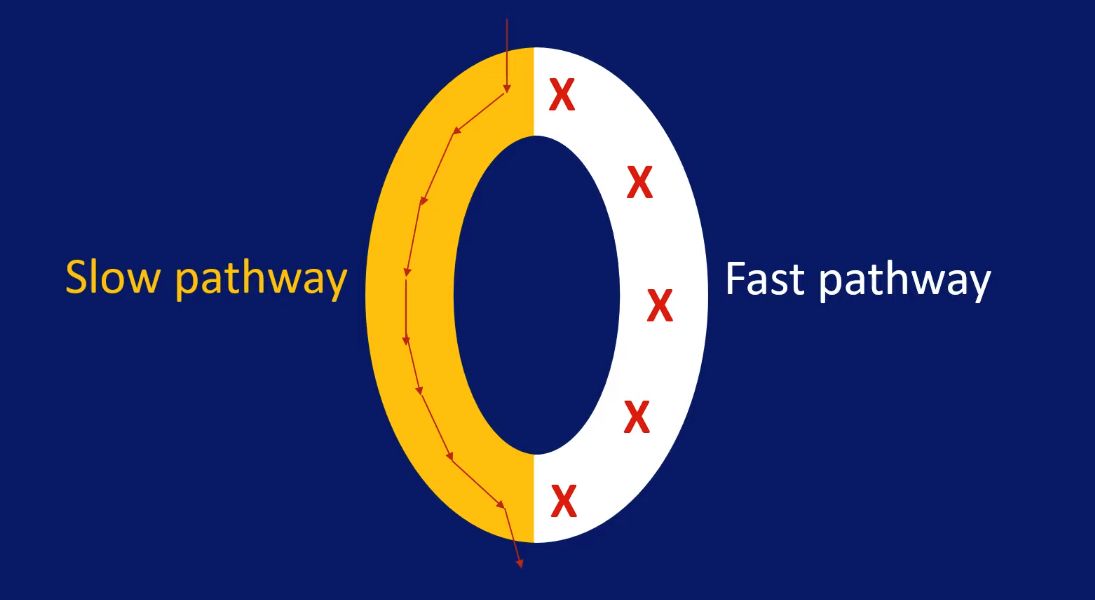
AVNRT depends on dual AV nodal pathways, the slow pathway and the fast pathway for the reentrant circuit. Fast pathway conducts faster but has longer refractory period and recovers later. Slow pathway has slower conduction but recovers earlier due to shorter refractory period. An appropriately timed atrial ectopic beat can find the fast pathway refractory and get conducted down the slow pathway. When it reaches the lower common pathway of the AV node, it finds that the fast pathway has recovered and gets conducted back into the atrium in addition to the ventricle, producing an AV nodal echo beat. This is the mechanism of re-entry in AVNRT.
When the atrial ectopic beat gets conducted down the slow pathway, there is a sudden increase in PR interval compared to the previous sinus beat. This is known as PR jump. PR jump has to be more than 50 ms to be significant. The monitor tracing given below illustrates the PR jump for the ectopic beat and an echo beat just after the QRS. Corresponding to the PR jump, during electrophysiology study, an AH jump can be demonstrated after an appropriately timed atrial extra stimulus.
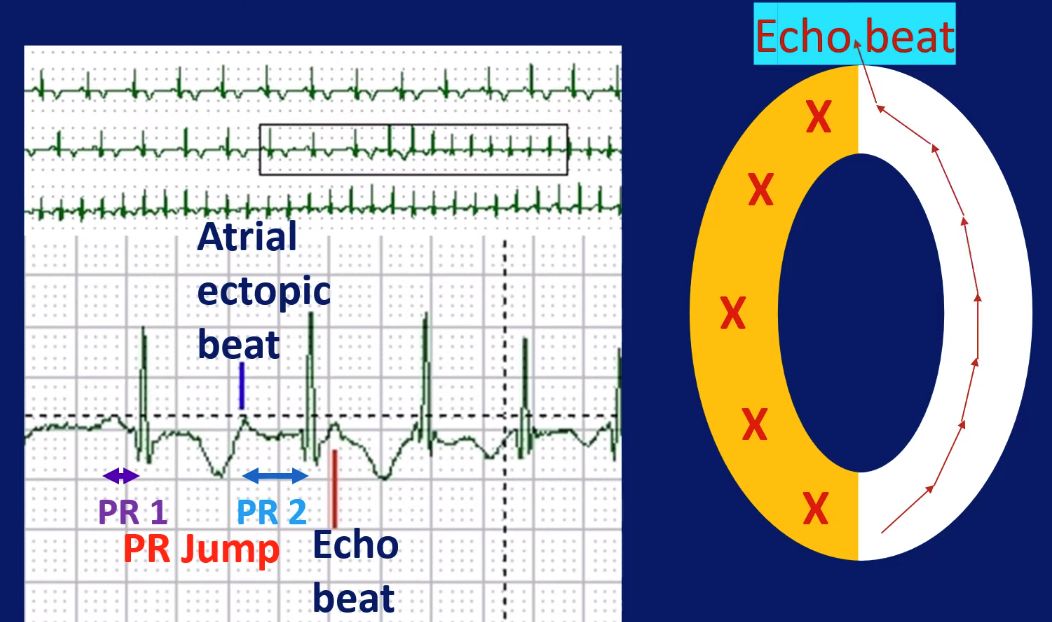
PR jump can also be induced by adenosine during sinus rhythm. In this case, PR jump is defined as a sudden increase in PR interval by 50 ms or more between two consecutive sinus beats. AV nodal echo is defined as a retrograde P wave at the end of the QRS complex as seen in the case of atrial ectopic in the previous ECG. Echo beat can also be followed by AVNRT, similar to what occurred after an atrial ectopic beat in the previous case. Thus adenosine is useful in demonstrating the presence of dual AV nodal physiology from surface ECG, which would indicate that the clinical tachycardia is AVNRT than AVRT. A positive adenosine test identified by a PR jump had a specificity of 94% and positive predictive value of 96% in one study [1].
References
- Toal SC, Vajifdar BU, Gupta AK, Vora AM, Lokhandwala YY. Adenosine induced PR jump on surface ECG to differentiate atrioventricular nodal re-entrant tachycardia from concealed accessory pathway mediated tachycardia: a bedside test. Heart. 2002 Jan;87(1):37-40. doi: 10.1136/heart.87.1.37. PMID: 11751662; PMCID: PMC1766948.
- Gupta A, Lokhandwala Y, Rai N, Malviya A. Adenosine-A drug with myriad utility in the diagnosis and treatment of arrhythmias. J Arrhythm. 2020 Dec 18;37(1):103-112. doi: 10.1002/joa3.12453. PMID: 33664892; PMCID: PMC7896475.
- Garratt CJ, Antoniou A, Griffith MJ, Ward DE, Camm AJ. Use of intravenous adenosine in sinus rhythm as a diagnostic test for latent preexcitation. Am J Cardiol. 1990 Apr 1;65(13):868-73. doi: 10.1016/0002-9149(90)91428-9. PMID: 2321537.

