Cardiotoxicities of antineoplastic medications
Cardiotoxicities of antineoplastic medications
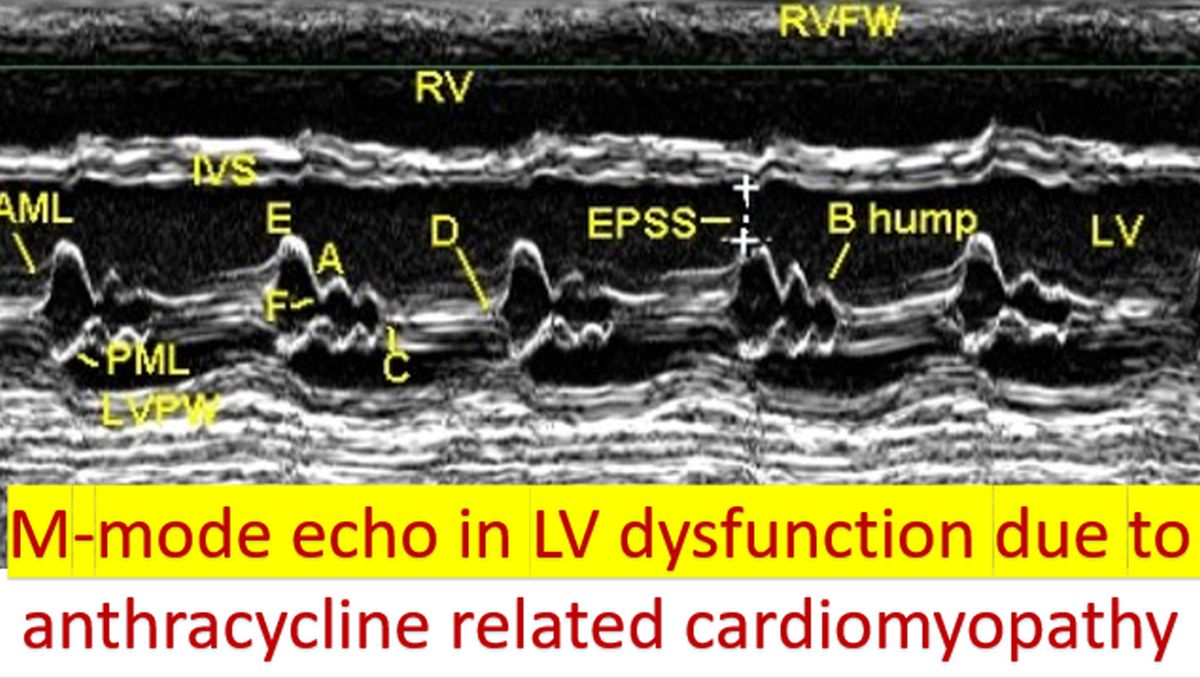
Anthracyclines like adriamycin and epirubicin are good chemotherapeutic agents which improve the long term survival, especially in breast cancer. But a small number of them develop cardiotoxicity, which is less with epirubicin than with doxorubicin (adriamycin) on a milligram per milligram basis. The chance for cardiotoxicity is more in the elderly and those with pre-existing heart disease. Concomitant radiotherapy and use of cyclophosphamide also increase the risk of adriamycin induced cardiomyopathy. The total cumulative dose is also an important determinant of risk. Conventional risk factors for heart disease like hypertension and diabetes mellitus also increase the risk of congestive heart failure with anthracycline therapy. One study found the risk of congestive heart failure with epirubicin to be about 5%. The risk becomes more significant in those with early stages of cancer who are likely to be cured of the illness.
Trastuzumab is useful for the chemotherapy of breast cancers which are HER2 (human epidermal growth factor receptor-2) positive, which constitute about one fifth of cases of breast cancer. Untreated, HER2 positive cases have a poorer prognosis than negative cases [1]. Adding trastuzumab as an adjuvant chemotherapeutic agent for one year has a significant impact on improving survival in HER2 positive breast cancer. There is a medium risk for development of cardiotoxicity with this monoclonal antibody. Most often it takes the form of asymptomatic left ventricular dysfunction documented on echocardiography while rarely clinical heart failure may also follow therapy with Trastuzumab. Severe heart failure / death is reported only in 0.6 to 4% in different studies. Risk is likely to be higher in those who have received doxorubicin therapy earlier.
Trastuzumab causes type II cardiotoxicity which may not be dose dependent, but reversible. HER2 receptors present on the myocytes may have role in cardiotoxicity [2]. Type I cardiotoxicity is irreversible and caused by death of cardiomyocytes, through necrosis or apoptosis. Type II cardiotoxicity may be reversible as it is caused by cardiomyocyte dysfunction and not cell death. Long term cardiotoxicity of anthracyclines is of type I with cell death mediated by free radical formation and hence likely to be irreversible [3].
Androgen deprivation therapies for prostate cancer are bilateral orchidectomy and gonadotropin-releasing hormone agonists. Androgen deprivation therapies can cause decreased muscle mass and increased fat mass, together known as sarcopenic obesity. In addition they can cause decreased insulin sensitivity and alterations in lipids. They have been associated with diabetes mellitus and cardiovascular disease risk [4].
Oral immunomodulatory drugs (IMiDs) thalidomide, lenalidomide and pomalidomide have a crucial role in the treatment of multiple myeloma. IMiDs, particularly thalidomide, is associated with increased risk of both venous and arterial thromboembolic events [5].
Proteasome inhibitors have significantly improved survival in patients with multiple myeloma. They have been rarely associated with serious cardiovascular complications like congestive heart failure, hypertension and arrhythmias. Highest rates of cardiotoxicity have been noted with carfilzomib. The evidence regarding cardiotoxicity of bortezomib is conflicting [6].
Immune checkpoint inhibitors are a promising group of novel anti cancer drugs. They are monoclonal antibodies targeting cytotoxic T lymphocyte-associated antigen 4 (CTLA-4), programmed cell death 1 (PD-1) and its ligand (PD-L1). Important drugs in this class are ipilimumab, nivolumab, pembrolizumab and atezolizumab. Autoimmune myocarditis which is potentially life threatening have been associated with immune checkpoint inhibitors [7].
Antimetabolite 5-fluorouracil can cause coronary vasospasm and ischemia. Life threatening cardiotoxicity is seen with a frequency less than 1%. Calcium antagonists like verapamil and nitrates may be useful in treatment of coronary spasm induced by 5-fluorouracil [8].

Vascular endothelial growth factor inhibitors have been associated with increased incidence of hypertension, ischemic heart disease, heart failure, QT interval prolongation and thromboembolism. Some important medications in this group are bevacizumab, ramucirumab, aflibercept, and sunitinib [9].
Tyrosine kinase inhibitors used in the treatment of chronic myelogenous leukemia can cause atherosclerosis and other vascular problems like coronary events, cerebrovascular events and peripheral vascular events [10]. Pulmonary arterial hypertension has been noted in patients treated by dasatinib [11].
Ibrutinib is a Bruton tyrosine kinase inhibitor effective against B-cell cancers. At the same time, it increases the risk of atrial fibrillation. Risk of atrial fibrillation has been attributed to inhibition of C-Terminal Src Kinase [12].
References
- Moja L, Tagliabue L, Balduzzi S, Parmelli E, Pistotti V, Guarneri V, D’Amico R. Trastuzumab containing regimens for early breast cancer. Cochrane Database Syst Rev. 2012 Apr 18;2012(4):CD006243. doi: 10.1002/14651858.CD006243.pub2. PMID: 22513938; PMCID: PMC6718210.
- Smith I, Procter M, Gelber RD, Guillaume S, Feyereislova A, Dowsett M, Goldhirsch A, Untch M, Mariani G, Baselga J, Kaufmann M, Cameron D, Bell R, Bergh J, Coleman R, Wardley A, Harbeck N, Lopez RI, Mallmann P, Gelmon K, Wilcken N, Wist E, Sánchez Rovira P, Piccart-Gebhart MJ; HERA study team. 2-year follow-up of trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer: a randomised controlled trial. Lancet. 2007 Jan 6;369(9555):29-36. doi: 10.1016/S0140-6736(07)60028-2. PMID: 17208639.
- Volkova M, Russell R 3rd. Anthracycline cardiotoxicity: prevalence, pathogenesis and treatment. Curr Cardiol Rev. 2011 Nov;7(4):214-20. doi: 10.2174/157340311799960645. PMID: 22758622; PMCID: PMC3322439.
- Faris JE, Smith MR. Metabolic sequelae associated with androgen deprivation therapy for prostate cancer. Curr Opin Endocrinol Diabetes Obes. 2010 Jun;17(3):240-6. doi: 10.1097/MED.0b013e3283391fd1. PMID: 20404727; PMCID: PMC5120548.
- Palumbo A, Palladino C. Venous and arterial thrombotic risks with thalidomide: evidence and practical guidance. Ther Adv Drug Saf. 2012 Oct;3(5):255-66. doi: 10.1177/2042098612452291. PMID: 25083240; PMCID: PMC4110867.
- Cole DC, Frishman WH. Cardiovascular Complications of Proteasome Inhibitors Used in Multiple Myeloma. Cardiol Rev. 2018 May/Jun;26(3):122-129. doi: 10.1097/CRD.0000000000000183. PMID: 29077585.
- Francis J, Abraham J. Immune Checkpoint Inhibitors and Myocarditis. BMH Med. J. 2019; 6(3):78-80.
- Alter P, Herzum M, Soufi M, Schaefer JR, Maisch B. Cardiotoxicity of 5-fluorouracil. Cardiovasc Hematol Agents Med Chem. 2006 Jan;4(1):1-5. doi: 10.2174/187152506775268785. PMID: 16529545.
- Touyz RM, Lang NN, Herrmann J, van den Meiracker AH, Danser AHJ. Recent Advances in Hypertension and Cardiovascular Toxicities With Vascular Endothelial Growth Factor Inhibition. Hypertension. 2017 Aug;70(2):220-226. doi: 10.1161/HYPERTENSIONAHA.117.08856. Epub 2017 Jun 19. PMID: 28630211; PMCID: PMC5509510.
- Manouchehri A, Kanu E, Mauro MJ, Aday AW, Lindner JR, Moslehi J. Tyrosine Kinase Inhibitors in Leukemia and Cardiovascular Events: From Mechanism to Patient Care. Arterioscler Thromb Vasc Biol. 2020 Feb;40(2):301-308. doi: 10.1161/ATVBAHA.119.313353. Epub 2019 Dec 26. PMID: 31875699; PMCID: PMC6993877.
- Montani D, Bergot E, Günther S, Savale L, Bergeron A, Bourdin A, Bouvaist H, Canuet M, Pison C, Macro M, Poubeau P, Girerd B, Natali D, Guignabert C, Perros F, O’Callaghan DS, Jaïs X, Tubert-Bitter P, Zalcman G, Sitbon O, Simonneau G, Humbert M. Pulmonary arterial hypertension in patients treated by dasatinib. Circulation. 2012 May 1;125(17):2128-37. doi: 10.1161/CIRCULATIONAHA.111.079921. Epub 2012 Mar 26. PMID: 22451584.
- Xiao L, Salem JE, Clauss S, Hanley A, Bapat A, Hulsmans M, Iwamoto Y, Wojtkiewicz G, Cetinbas M, Schloss MJ, Tedeschi J, Lebrun-Vignes B, Lundby A, Sadreyev RI, Moslehi J, Nahrendorf M, Ellinor PT, Milan DJ. Ibrutinib-Mediated Atrial Fibrillation Attributable to Inhibition of C-Terminal Src Kinase. Circulation. 2020 Dec 22;142(25):2443-2455. doi: 10.1161/CIRCULATIONAHA.120.049210. Epub 2020 Oct 23. PMID: 33092403.