Clinical Examination of Cardiovascular System For Medical Students
Clinical Examination of Cardiovascular System For Medical Students
This lecture gives a comprehensive coverage of cardiovascular system including inspection, palpation, percussion, and auscultation.
Clinical examination is guided by the symptoms. Unless the history is correlated with physical findings, important diagnostic possibilities may be missed. Clinical examination starts off with a focused general examination followed by a detailed examination of the cardiovascular system.
Relevant points in other systems like basal crepitations, hepatosplenomegaly and neurological deficits should be looked for. Examination strategy should be fitting to the clinical situation. When a patient presents to the emergency room, it should be a short but focused examination to permit early initiation of emergency management.
While the examination in emergency room is a short and focussed one, that on the floor or elsewhere should be a detailed examination, trying to unearth all possible differential diagnoses to plan further investigations and management.
Now we will move on to the general examination with respect to the cardiovascular system.
General appearance of the person will give you an idea on whether emergency management is needed or not. Do not wait for detailed evaluation if the person is moribund. Start resuscitatory measures along with your assessment. General examination can proceed in a head to foot order so that important points are not missed.
As part of general examination, eyes have a lot of information in relation to cardiovascular disorders. Look for pallor, jaundice, cyanosis, and polycythaemia. The last two are seen in congenital cyanotic heart disease. Squint with ocular muscle weakness, a feature of Kearns-Sayre syndrome may be associated with complete heart block.
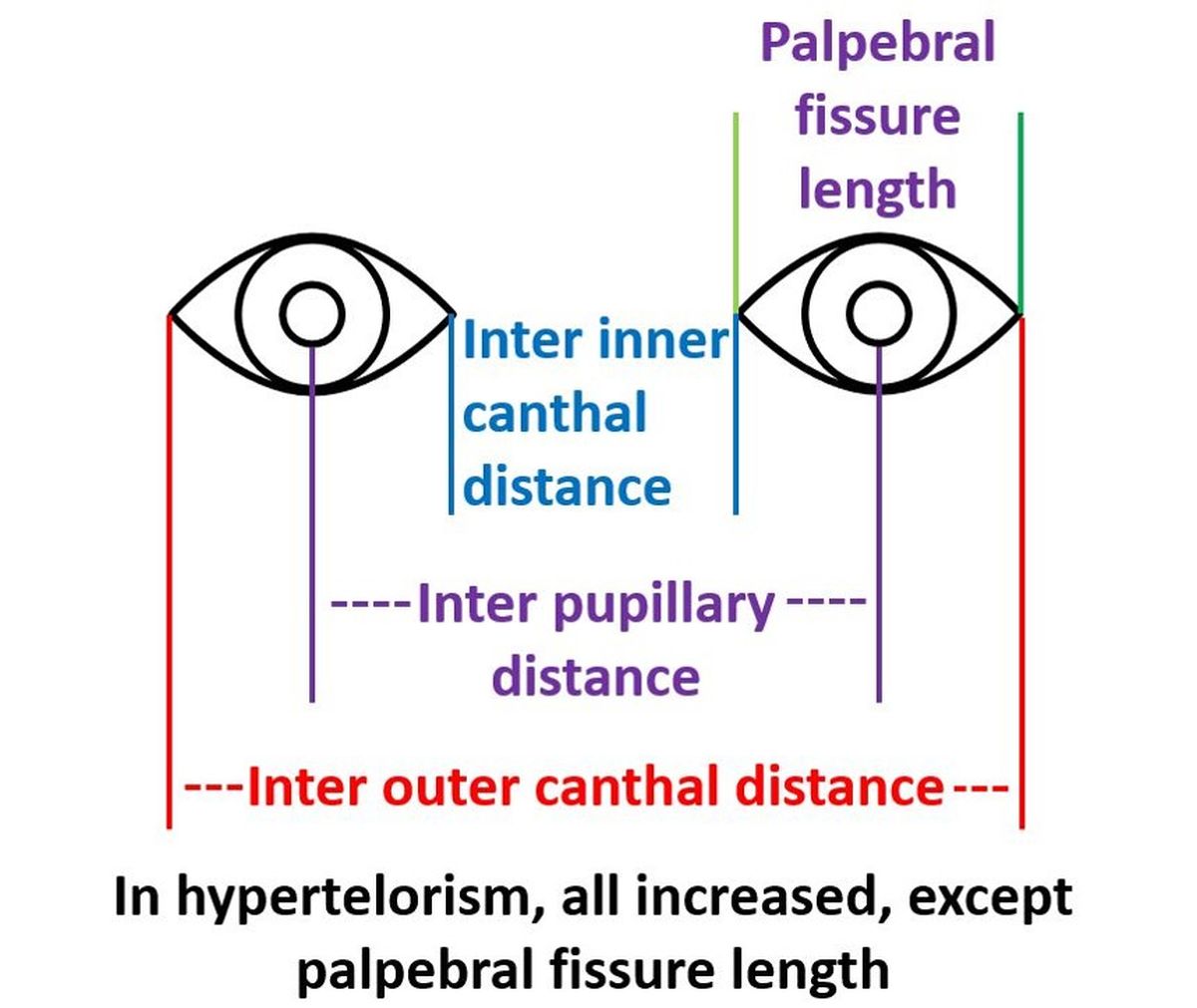
Hypertelorism and epicanthal folds are noted in Down syndrome. Cataract is seen in congenital rubella syndrome with patent ductus arteriosus or peripheral pulmonary stenosis.
Epicanthal folds and ptosis also come under facial dysmorphism, along with down sloping palpebral fissures and can be seen in Noonan syndrome associated with pulmonary stenosis.
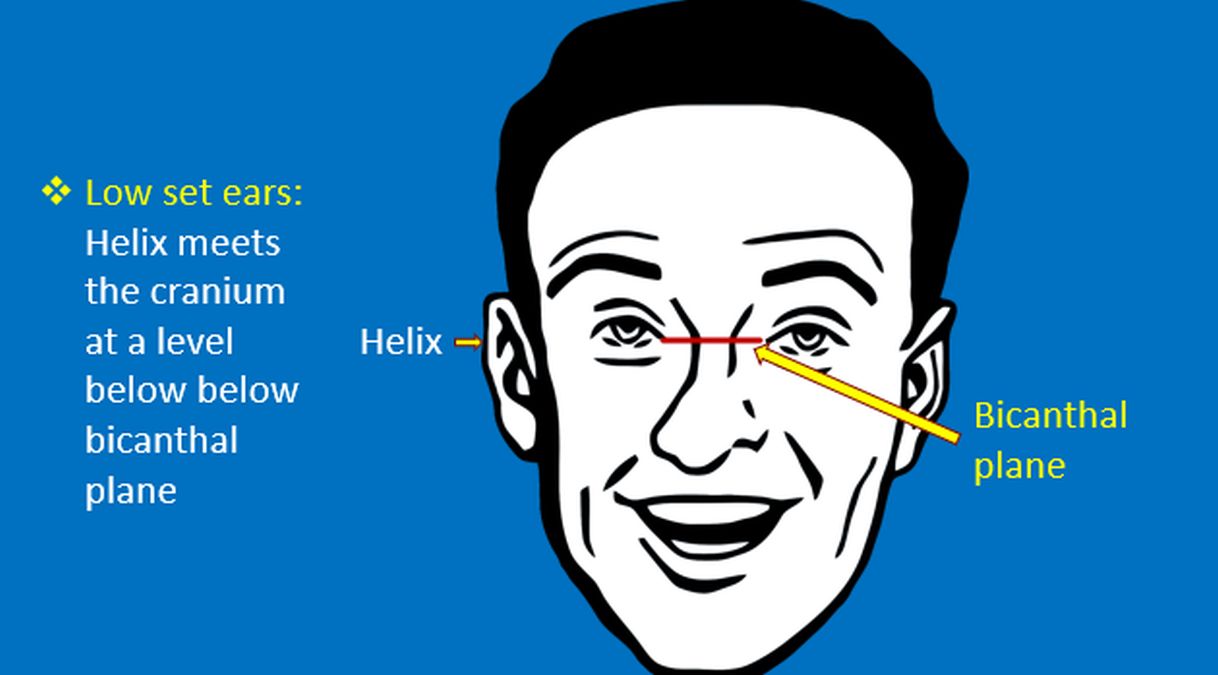
Low set ears can be seen in Noonan syndrome, Down syndrome and Di George syndrome. Latter two are associated with different types of cardiovascular defects. Noonan syndrome is associated with pulmonary stenosis.
Webbing of neck is seen in Turner syndrome and Noonan syndrome (sometimes called male Turner syndrome though it occurs in both males and females). Turner syndrome is associated with coarctation of aorta.
Cleft lip and palate have been associated with multiple types of cardiac defects including ventricular septal defect, tetralogy of Fallot and tricuspid atresia. Facial dysmorphism is also a feature in Andersen-Tawil syndrome, a type of long QT syndrome with inherited arrhythmias and periodic paralysis.
High arched palate is a feature in Ehlers-Danlos Syndrome and Marfan syndrome. Both can be associated aortic root dilatation and aortic regurgitation.
Cyanosis and pallor can be noted in the tips of the digits. Severe jaundice may be visible in the palms and soles, especially in small infants.
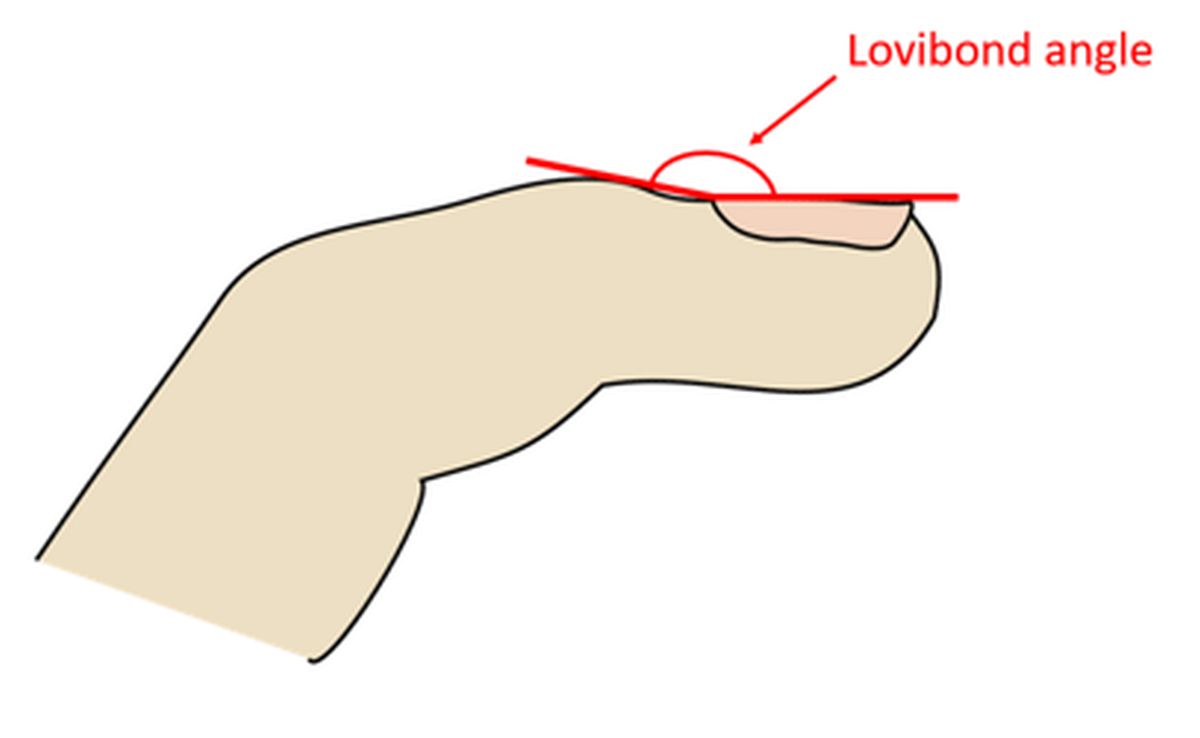
Clubbing of digits may be noted in cyanotic heart diseases, infective endocarditis as well many other noncardiac conditions. In clubbing, initially there is increased fluctuation of the nail bed, that is grade 1, followed by obliteration of angle between nail and the adjacent skin fold or the Lovibond angle, that is grade 2. Later there is increase in the curvature of the nails, known as parrot beaking, that is grade 3.
Grade 4 or hypertrophic osteoarthropathy is not common in cardiovascular causes of clubbing, hence the term hypertrophic pulmonary osteoarthropathy. It is a triad of periostitis, digital clubbing and painful arthropathy of the large joints, classical of lung cancer.
Osler’s nodes are tender reddish spots on the distal aspects of the fingers and toes, noted in infective endocarditis. Janeway lesions are nontender erythematous patches on the palms and soles, seen in in infective endocarditis. Splinter haemorrhages are linear streaks in the nail bed, typically seen in infective endocarditis, though it can also occur with trauma.
Arachnodactyly or long slender digits resembling those of arachnids, that is the spider family, is a feature of Marfan syndrome. Polydactyly with extra digits is part of Ellis-Van Creveld syndrome which has in addition short stature and cyanotic congenital heart disease like single atrium.
Edema is collection of fluid in the subcutaneous tissue. If it is unilateral, the cause is local like lymphedema or deep vein thrombosis, that is clotting of blood in deep veins of the legs. Pitting edema is demonstrated by sustained pressure over the lower part of tibia to displace the fluid and form a pit.
Bilateral pitting edema which is usually pitting in nature, can occur in cardiac failure, renal failure, and hepatic failure. Hypoproteinemia and hypothyroidism are other important causes. Long standing edema can become nonpitting in nature.
Now from general examination, we move on to the examination of the cardiovascular system.
Evaluation of pulse though part of general examination, is considered here in the examination of cardiovascular system in detail. Discussion on blood pressure is not included here as a separate topic is dedicated to it.
Though the most commonly examined pulse is the radial, to check some of the characteristics, a more proximal pulse like the brachial or carotid needs to be examined. Following parameters of the pulse are routinely documented: 1. The rate: Normal rate in adult is 60-100 per minute. It is higher in children. Younger the child, higher the pulse rate.
- Rhythm: Regular and irregular rhythms are possible. Mild variation with respiration is called respiratory sinus arrhythmia, with higher rate in inspiration. Respiratory sinus arrhythmia may be exaggerated in children. If the rhythm is totally irregular, it is likely to be atrial fibrillation. Patterned irregularity like pulsus bigeminus can occur due to ectopic beats or second degree atrioventricular block.
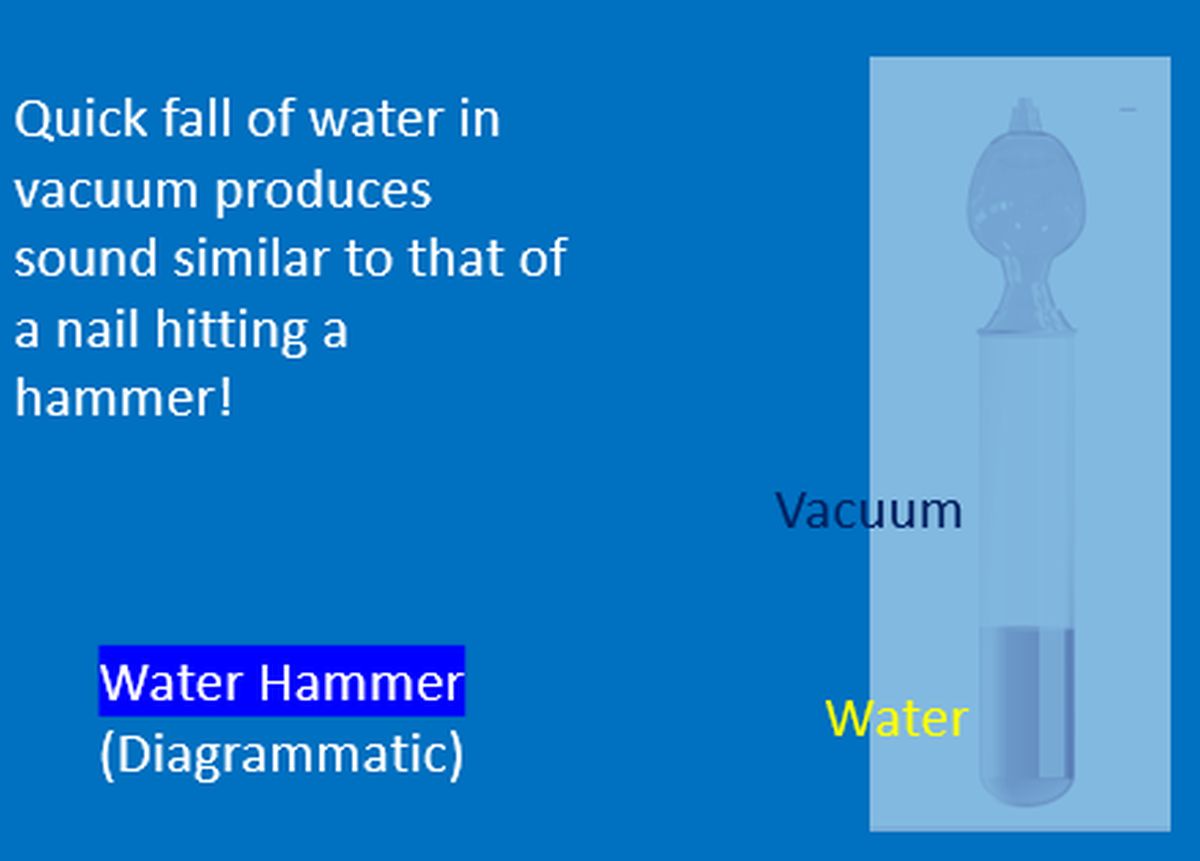
- Volume: Low volume pulse is noted in shock and severe aortic stenosis (Pulsus parvus). High volume pulse is felt in aortic regurgitation. 4. Character: A slow rising pulse is seen in aortic stenosis (Pulsus tardus). Collapsing pulse or water hammer pulse is a feature of severe aortic regurgitation. Water hammer was a toy in the Victorian period. Collapsing character of the pulse is better appreciated with the palm and having upper limb raised above the head.
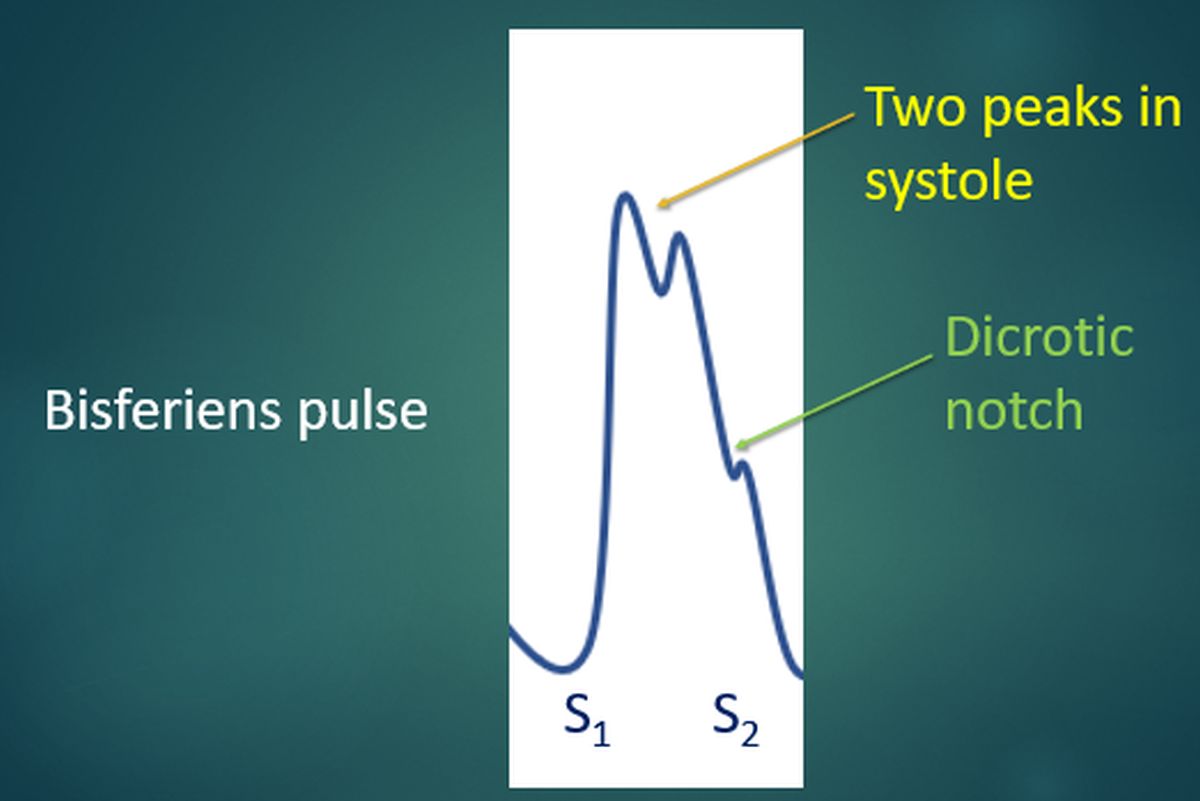
A bifid pulse with two peaks in systole is known as bisferiens pulse. It is noted in free aortic regurgitation and with a combination of aortic stenosis and aortic regurgitation.
Pulsus paradoxus is an exaggeration of the inspiratory fall in pulse volume, characteristic of cardiac tamponade. Pulsus alternans, a feature of left ventricular failure, is the beat to beat alternation in pulse volume.
- Vessel wall: Palpable vessel is a feature of arteriosclerosis in elderly. It can be felt by Osler’s manoeuvre using three fingers at the radial pulse known as trisection. Index and ring fingers occlude the vessel proximally and distally while the middle finger palpates the vessel wall. Alternate method is to occlude the brachial artery with one hand and palpate the radial vessel wall with the other hand.
A palpable radial artery after brachial occlusion, better done by inflation of a blood pressure cuff on the arm, constitutes the Osler’s sign. It is usually associated with pseudohypertension. 6. Peripheral pulses including radiofemoral/brachiofemoral delay: All peripheral pulses should be checked and documented. Some may be absent in peripheral arterial disease and aortic dissection.
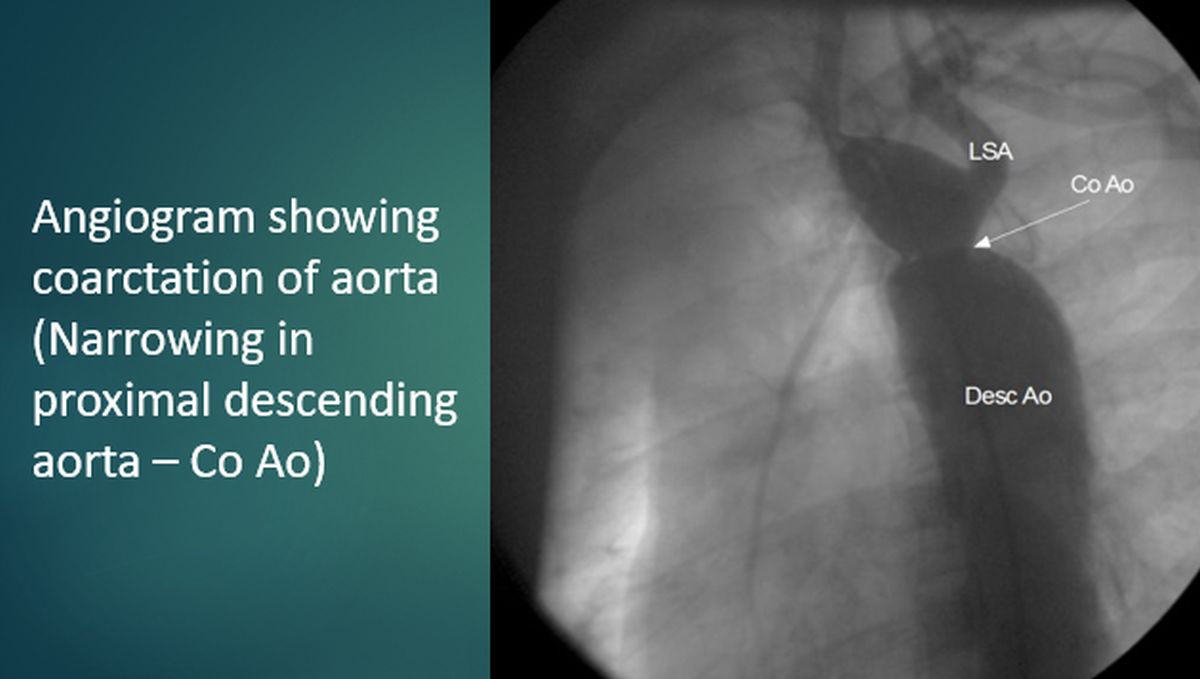
Radiofemoral/brachiofemoral delay is a feature of coarctation of aorta and it is associated with weak lower limb pulses. Normally femoral pulse is slightly earlier than radial pulse. Brachioradial delay has been considered to be an indicator of severity of aortic stenosis.
Now we move on to assessment of jugular venous pulse and pressure. Assessment of jugular venous pulse has to be done in the internal jugular vein though a beginner is often tempted to use the external jugular vein. External jugular vein may be kinked, and it may not reflect the true right atrial pressure. Jugular venous pressure is measured with reference to the sternal angle.
The sternal angle is 5 cm above the mid right atrium in all positions. Normal internal jugular venous pulsations are not visible in the neck in the sitting position. Hence it is typically measured with 45 degrees propped up position. But if the venous pressure is elevated, measurement in sitting position is possible.
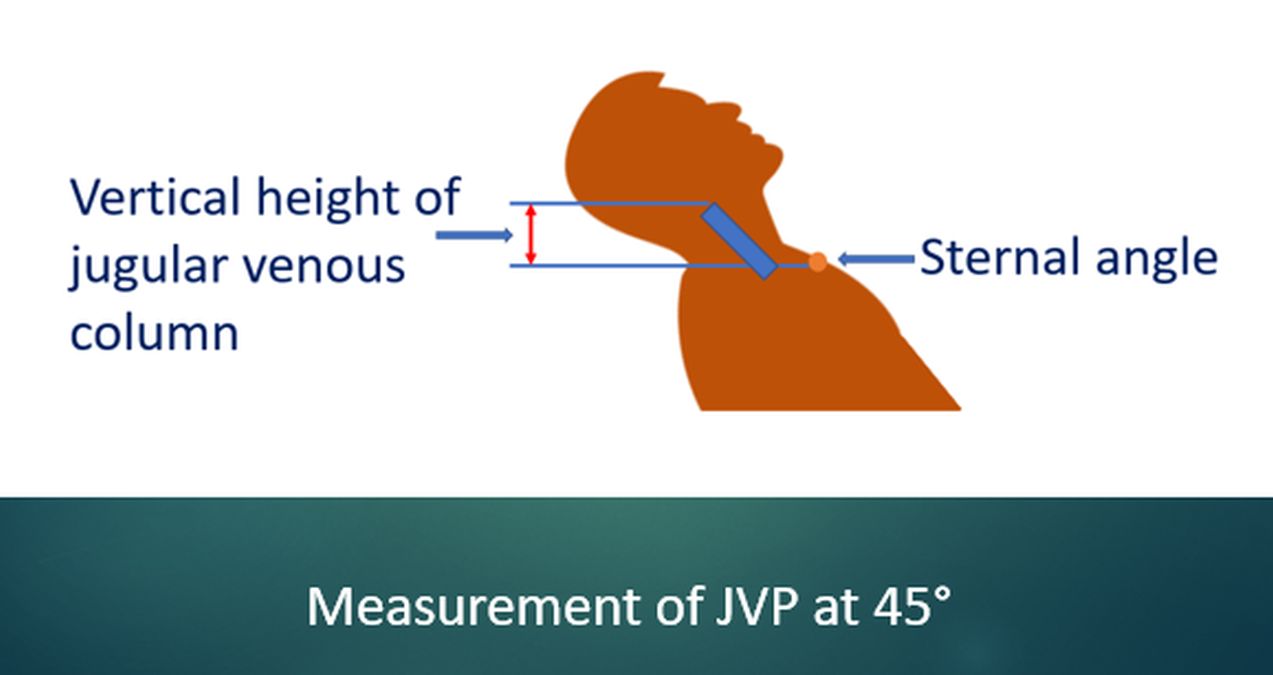
Vertical distance of the upper level of the pulsations above the sternal angle is noted and measured in centimetres of jugular venous pressure. Sometimes the JVP may be so high that the upper level may not be visible. It may be visible in standing position in such cases. Pulsations of the ear lobe will be noted in such cases.
In cases without visible elevation of JVP, sustained pressure over the upper abdomen for 30 seconds may be given to elicit the abdominojugular or hepatojugular reflux. While examining engorged jugulars, it is important to check whether they are pulsatile or non-pulsatile. Non-pulsatile engorged jugulars suggest superior vena caval obstruction, the superior vena cava syndrome.
Respiratory variation of the jugular venous pulsations is another important aspect. Normally the amplitude of the pulsations increase in inspiration while the upper level, that is the jugular venous pressure, falls in inspiration as the blood rushes into the right atrium. An inspiratory increase in jugular venous pressure is known as Kussmaul’s sign. It is seen in right heart failure and is a typical sign in constrictive pericarditis.
An often asked question is how to differentiate between venous and arterial pulsations in the neck. The usual answer is: Venous pulsations are better seen than felt. Venous pulsation has a definite upper level. Venous pulsation has multiple waves in a cardiac cycle while the arterial pulsation usually has only a single wave.
Jugular venous pulse tracing resembles right atrial pressure tracing. It has three positive waves: a, c and v and two negative waves: x and y descents.
During clinical examination, the descents are better appreciated than the waves, of which y descent is the most prominent. On visual inspection, only a and v waves are visible while c wave can be documented only in a pulse recording.
a wave is due to atrial contraction. It is prominent in tricuspid stenosis, pulmonary stenosis and pulmonary hypertension, when the atrial contraction is more forceful. Presence of an a wave excludes an unrestricted ventricular septal defect. Intermittent large a waves may be seen in complete heart block when atrial contraction occurs with a closed tricuspid valve. These are called cannon waves. a wave is absent in atrial fibrillation as there is no organized atrial contraction.
c wave in jugular venous pressure is a carotid artifact. In the atrial pressure tracing it is due to bulging of the atrioventricular valve during ventricular contraction.
v wave occurs during venous filling after the ventricular contraction. In tricuspid regurgitation, c and waves fuse together to form a prominent cv wave. It is also called just a prominent v wave.
x descent is absent in tricuspid regurgitation. Y descent can be prominent in constrictive pericarditis and is known as Friedreich’s sign. y descent is shallow in tricuspid stenosis and in cardiac tamponade, the y descent is absent.
Precordial examination starts with inspection, though inspection and palpation are often combined in regular practice. Some of the features to look for are: sternal deformities like pectus excavatum, which is a concavity of the sternum and is the commonest congenital malformation of the chest wall which may be associated with congenital heart diseases like ventricular septal defect.
Pectus carinatum is sternal prominence, also known as pigeon chest, which can occur in congenital heart disease with large left to right shunts in infancy. Second, visible pulsations: Suprasternal pulsations can be seen in aortic aneurysm and aortic regurgitation. A large dilated pulmonary artery can cause pulsation in the second left intercostal space.
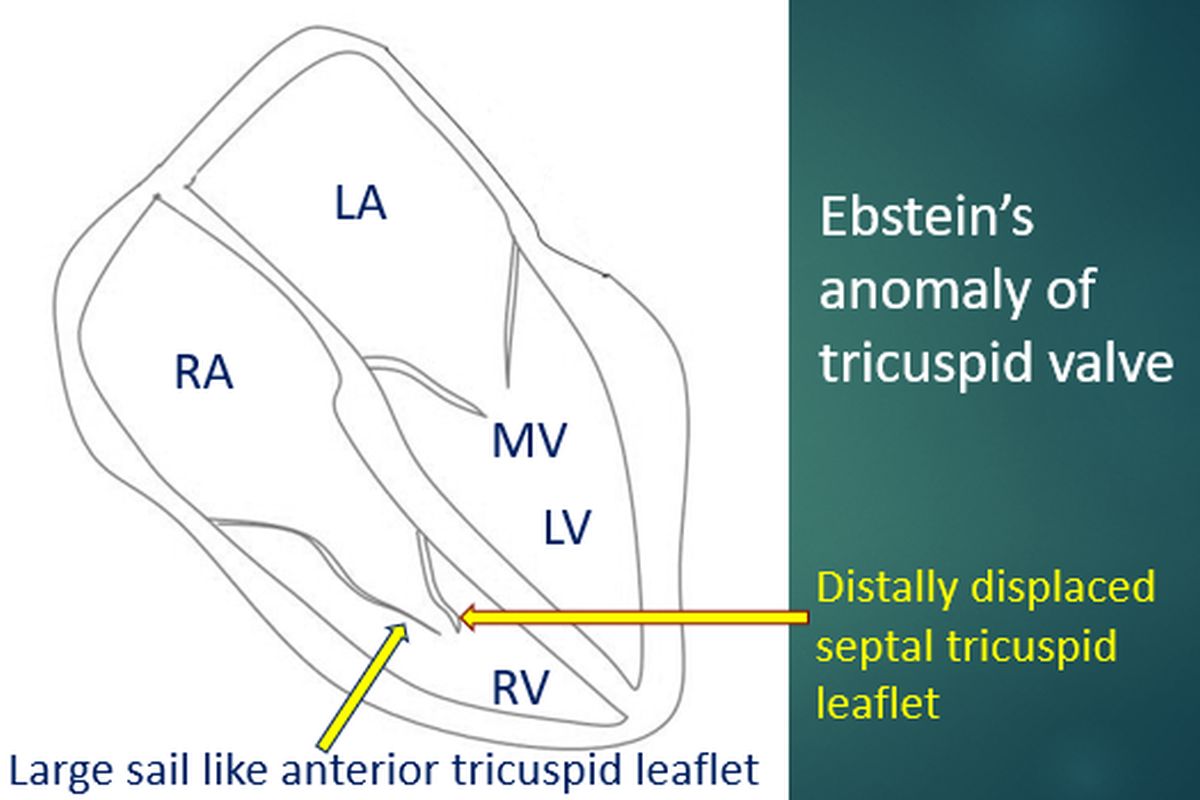
Left parasternal pulsations can be seen in right ventricular enlargement. Grossly enlarged left atrium with mitral regurgitation and dilated right ventricular outflow tract in Ebstein’s anomaly are other rare causes of left parasternal pulsations.
Right ventricular outflow tract pulsations in Ebstein’s anomaly are often better seen than felt. It is a wavy pulsation. Similar right ventricular outflow tract pulsations may be seen in right ventricular endomyocardial fibrosis as well. Enlarged right ventricle can also cause epigastric pulsations.
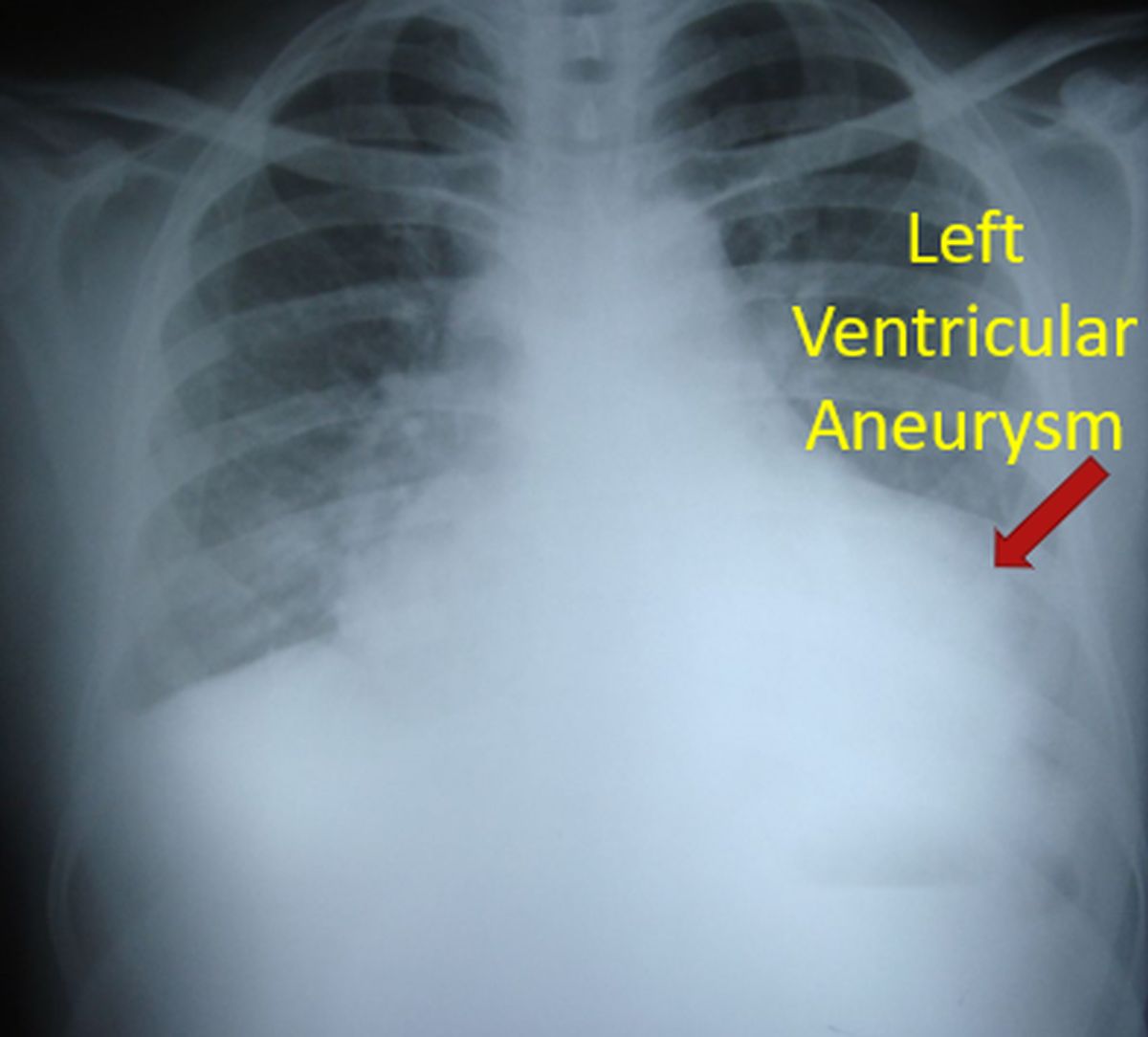
Pulsations above the apical impulse are noted in left ventricular aneurysm. Submitral left ventricular aneurysms can also cause pulsations on the left cardiac border. Right parasternal pulsations may occur with grossly dilated aortic root.
Third category is surgical scars. Midline sternotomy scar is probably the commonest in the adult and can be after coronary artery bypass grafting or valve replacements. Anterolateral thoracotomy scars are noted after a closed mitral valvotomy and some pericardial surgeries.

Posterolateral thoracotomy scars are seen after surgeries on great vessels like closure of patent ductus arteriosus and repair of coarctation of aorta. Fourth category are the dilated veins. Dilated veins can occur with obstruction of superior or inferior vena cava. The direction of blood flow in the dilated veins will be downwards in superior vena cava obstruction and upwards in inferior vena cava obstruction.
Five: Dilated arteries: Dilated intercostal arteries and anastomosis around the scapula may be visible in coarctation of aorta. But they are often better felt than seen. Apex beat is better characterized by palpation, though it is often visible.
Now we will move on to palpation of precordium and adjacent areas.
Palpation initially confirms the findings of inspection and further looks for new findings. One Apex beat: Apex beat is defined as the lowest and outer most point of definite cardiac impulse. If apex beat is not felt on left side, immediately check on the right side or else we might miss a dextrocardia. There are some who even palpate both sides simultaneously for this reason.
Apex beat is initially felt with the palm of the hand and then localized with the index finger. Sometimes it may be difficult to palpate in obese individuals and in those with emphysema. Palpation in held expiration and in the left lateral position may help in localization. Normal apex beat is felt in the 5th left intercostal space, typically about 1 cm medial to the mid clavicular line.
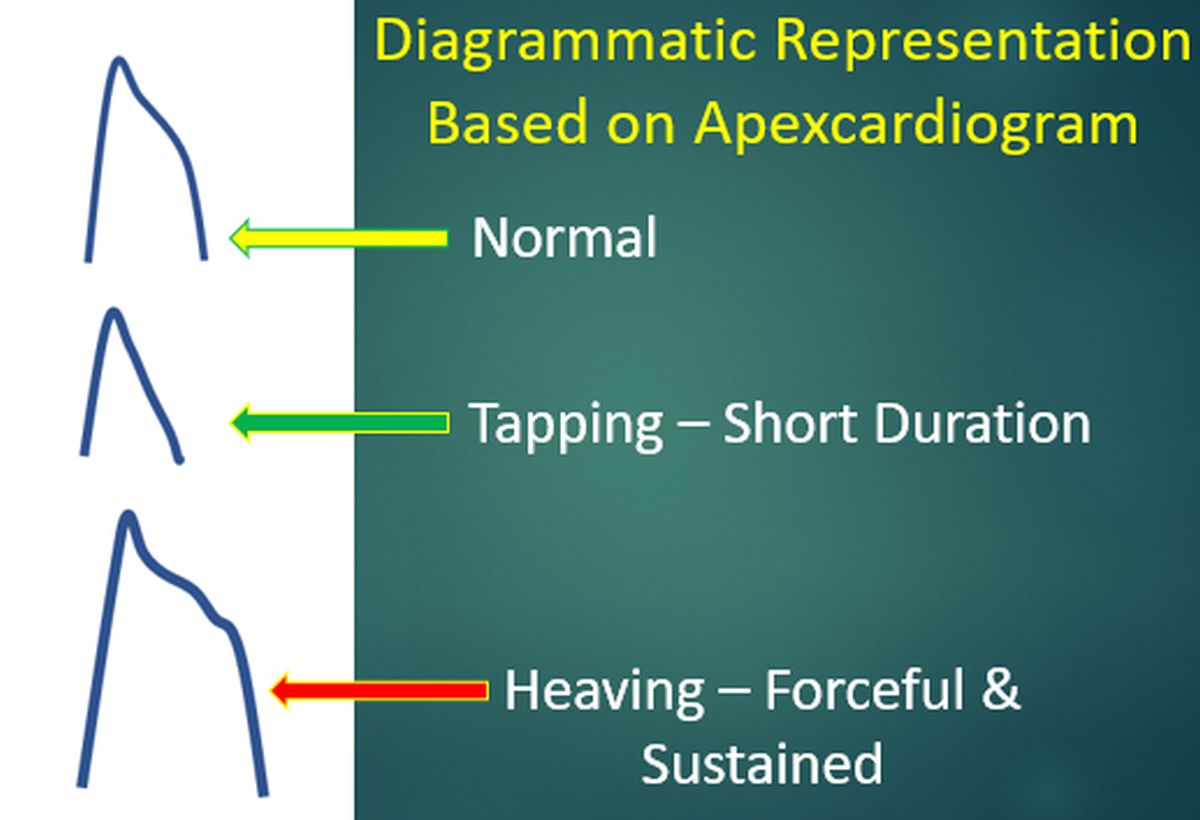
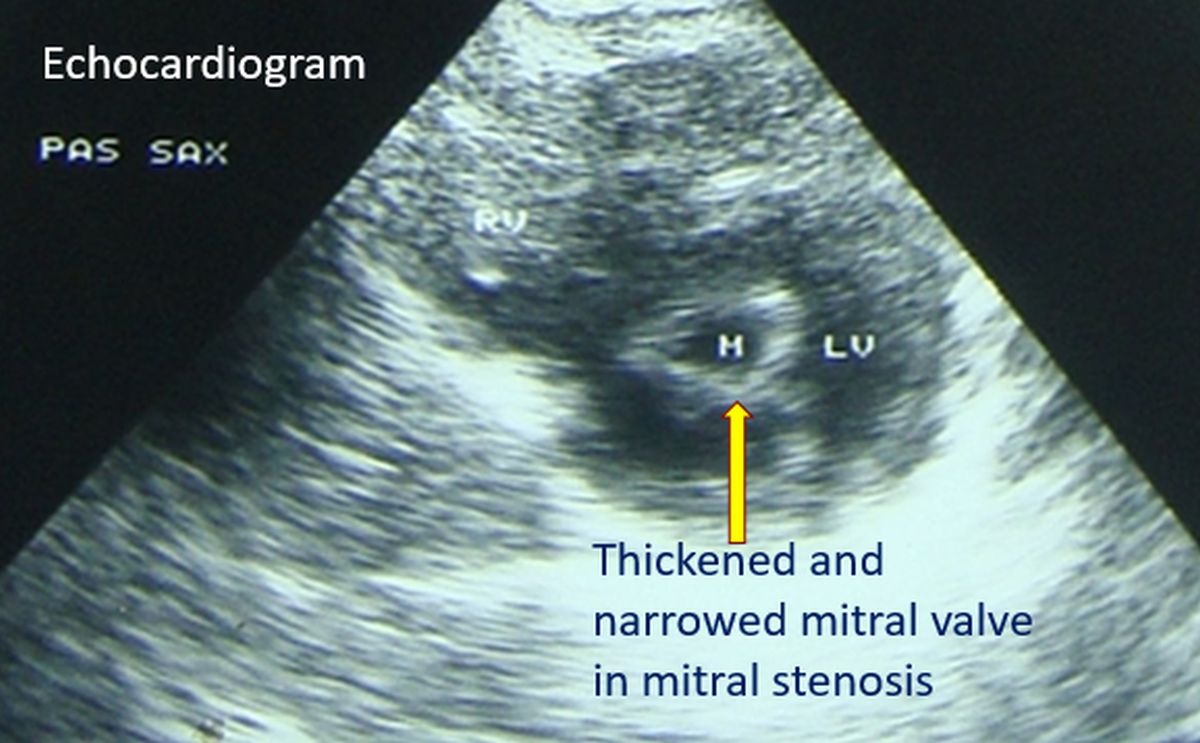
Tapping apex beat is the palpable counterpart of a loud first heart sound in mitral stenosis. A forceful apex beat is seen in regurgitant lesions like aortic and mitral regurgitation. It is also called a hyperdynamic apex. Heaving apex beat is both forceful and sustained and is characteristic of left ventricular hypertrophy of severe aortic stenosis.
Dyskinetic apex in left ventricular aneurysm is a see-saw pulsation with an additional out of phase bulge above the lowest impulse. Point of maximum impulse is sometimes checked when the apical impulse is diffuse and difficult to localize. Pulse – apex deficit is a term used in atrial fibrillation to note the difference between the pulse rate and the rate of apical impulses.
Pulse deficit is usually more than 10 per minute in atrial fibrillation as all beats may not have a good pulse in the fast irregular rhythm. Double apical impulse and triple apical impulse may be felt in hypertrophic obstructive cardiomyopathy. In hypertrophic obstructive cardiomyopathy, one of the impulses may be diastolic, being the palpable component of a loud fourth heart sound due to forceful atrial contraction.
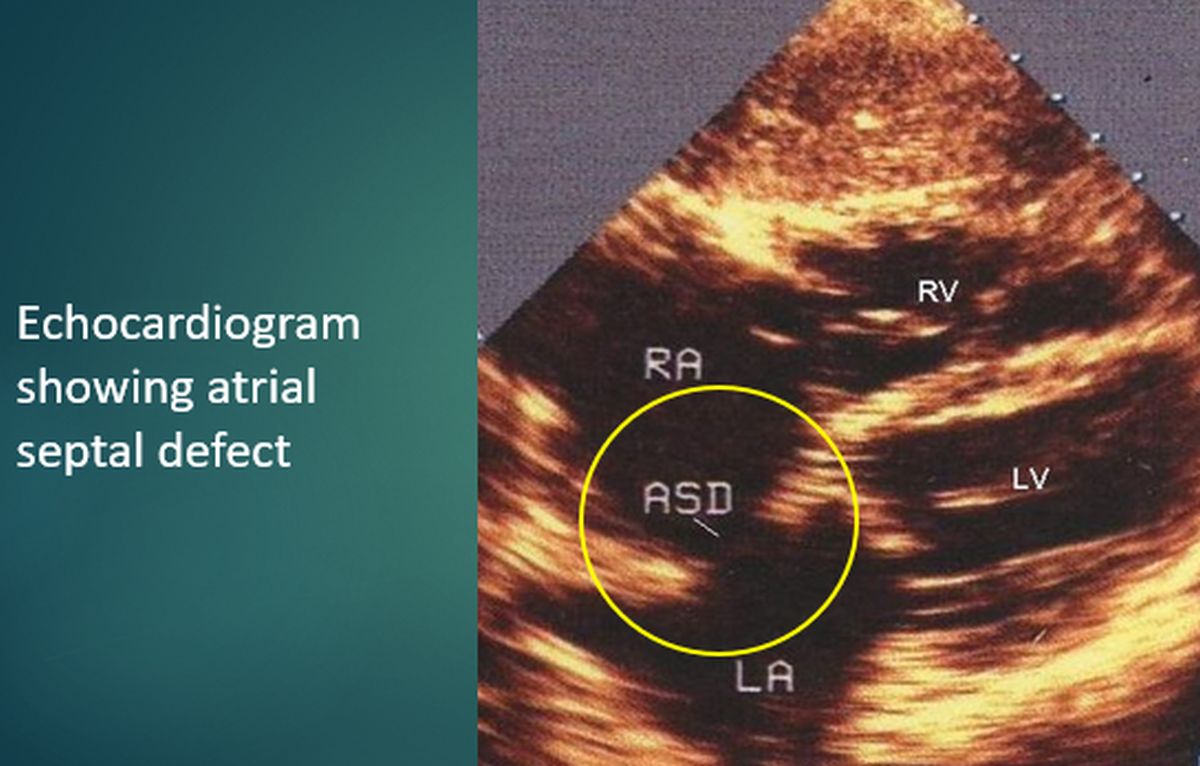
Left parasternal heave: Left parasternal heave is felt with the ulnar aspect of the palm which is kept perpendicular to the precordium. It is a feature of right ventricular hypertrophy. Hyperdynamic left precordial pulsations which are not so forceful can be noted in atrial septal defect with large left to right shunt even without severe pulmonary hypertension and right ventricular hypertrophy.
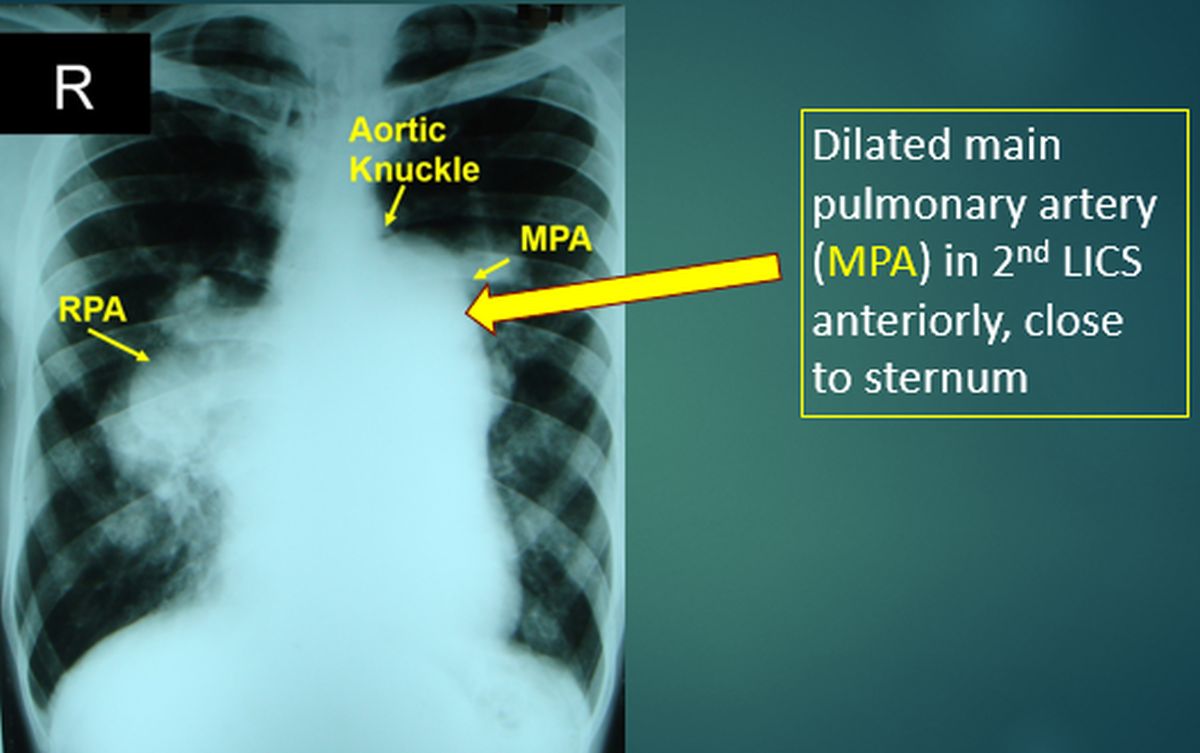
Pulsations in second left intercostal space: Pulsations in left intercostal space indicate enlarged pulmonary artery, are better felt with the fingertips, after flexing the proximal interphalangeal joints at right angle. Right parasternal pulsations may be noted if the aortic root is grossly dilated.
Hepatic pulsations are better felt by bimanual palpation with one hand over the right hypochondrium and another over the back. Presystolic pulsations are noted in tricuspid stenosis and systolic pulsations in tricuspid regurgitation. Suzman sign is the visible or palpable collaterals in the upper back in coarctation of aorta. They are seen better on bending forward.
Thrills are the palpable counterparts of cardiac murmurs and are generally associated with very loud murmurs, grade IV and above. Thrills are better appreciated with the ulnar aspect of the palm of the hand. Location and timing of thrill depends on the cause. Thrills can be systolic, diastolic or continuous. They can be timed with respect to the carotid pulse, just like murmurs.
Thrill of aortic stenosis can be felt in the second right intercostal space or the left parasternal region.
In pulmonary stenosis, it is present in the second left intercostal space.
Both these are systolic thrills.
Thrill of small ventricular septal defect (maladie de Roger) is systolic and noted in the left parasternal region.
Systolic thrill of mitral regurgitation is felt at the apex.
Diastolic thrill of mitral stenosis is highly localized to the apex.
Diastolic thrill may occur in aortic regurgitation in the left parasternal region.
Continuous thrill in the first and second left intercostal space is noted in patent ductus arteriosus.
Now we move on to percussion of the precordium.
Percussion is used only in limited scenarios currently. Three important aspects of percussion are:
1.Left border corresponds to apex beat: If there is dullness beyond the apex beat, it indicates pericardial effusion. But it may be difficult to palpate the apex beat in severe pericardial effusion.
2.Right heart border within right sternal edge: Dullness beyond right sternal edge may indicate right atrial enlargement in the lower part and aortic root dilatation in the upper part. It is necessary to percuss out the upper border of liver before eliciting this sign.
3.Dullness of 2nd left intercostal space close to sternum: Dullness in 2nd left intercostal space usually occurs in severe pulmonary hypertension with dilated pulmonary artery. It may be noted that a mass in this region can also produce dullness.
Precordium is generally divided into four auscultatory areas, but other areas may be checked in specific situations. The common auscultatory areas correspond to the locations at which the corresponding valvular events are better heard.
- Aortic area: Also called primary aortic area as there is a secondary aortic area along the left sternal edge. Primary aortic area is the 2nd right intercostal space, close to sternum. 2. Pulmonary area: 2nd left intercostal space, close to sternum.
- Tricuspid area: Lower left sternal edge, medial to apex beat. 4. Mitral area: At the apex beat, usually within the mid clavicular line in the 5th left intercostal space.
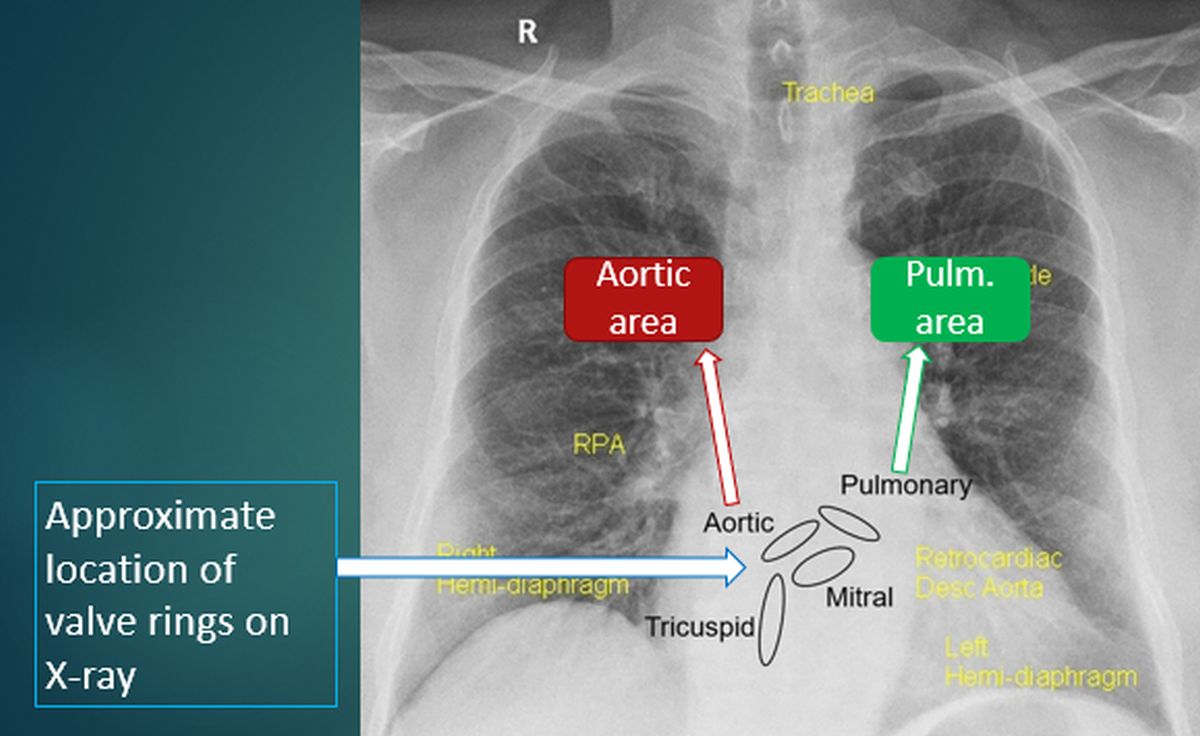
Other auscultatory areas can be used in specific situations, though not in routine clinical examination of all cases: 1. Erbs’s area: Third left intercostal space, close to sternum, where the murmur of aortic regurgitation may be better heard. This region is also called secondary aortic area.
- Roger’s area: Fourth left intercostal space, close to sternum where the murmur of small ventricular septal defect (maladie de Roger) is heard. In addition to these certain regions are auscultated when specific lesions are suspected:
- Infraclavicular region (1st left intercostal space): The murmur of patent ductus arteriosus may be best heard here. 2. Interscapular, scapular and infrascapular regions: Collateral murmurs and the bruit of coarctation of aorta may be checked for in these regions.
- Carotids: Murmur of aortic stenosis radiates to the carotids. Selective radiation to right carotid indicates supravalvular aortic stenosis. Carotid bruit can occur in carotid stenosis due to atherosclerosis and predisposes to stroke. Bruit is the vascular counterpart of murmur.
- Axilla: Murmur of mitral regurgitation radiates to the axilla and back. This is usually a feature seen in rheumatic mitral regurgitation with predominant involvement of anterior mitral leaflet. In papillary muscle dysfunction usually the posterior leaflet is involved and the mitral regurgitation murmur radiates medially and to the base of the heart rather than to the axilla.
Now we move on to the heart sounds. Two normally heard heart sounds are the first heart sound (S1) and second heart sound (S2). Second heart sound has two components – aortic (A2) and pulmonary (P2). Normal A2 is heard in all auscultatory areas while normal P2 is heard only in the pulmonary area. If it is heard at the apex, it can be considered as loud P2.
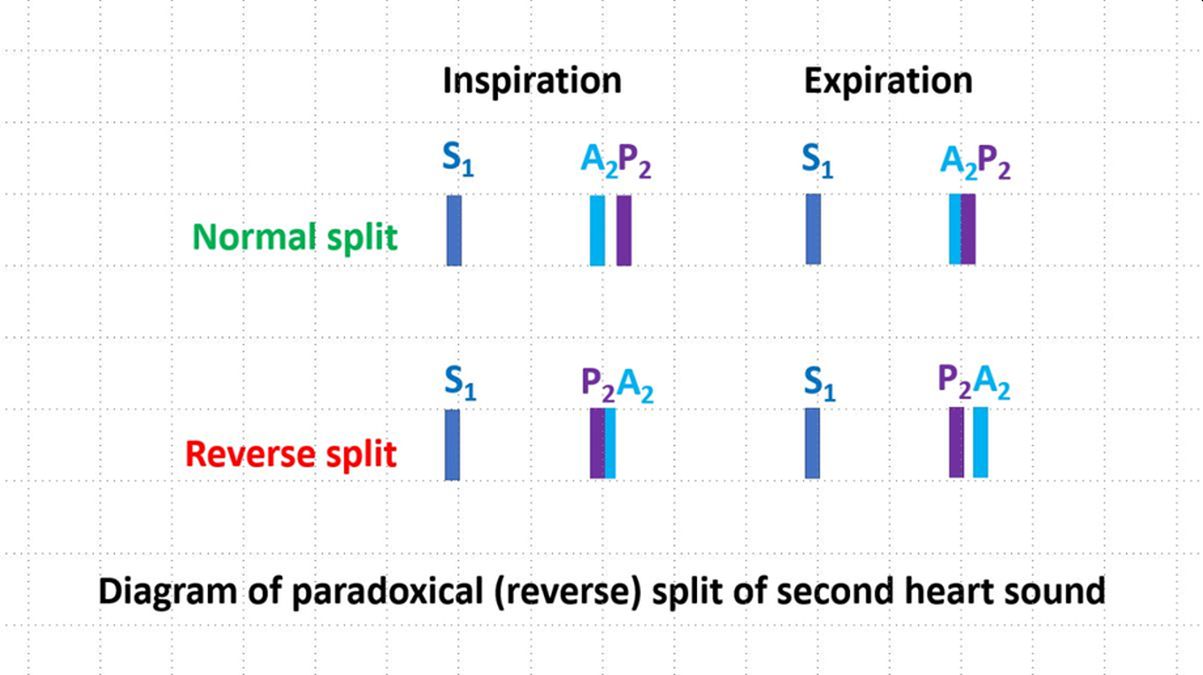
Normal split of second heart sound closes in expiration and is audible only in inspiration. If it is audible in both inspiration and expiration, it is called wide split. If the split increases in expiration and closes in inspiration, it is paradoxical split. Wide fixed split is audible in both inspiration and expiration, without any change in the A2-P2 interval.
Third and fourth heart sounds are usually heard in pathological conditions. But a third heart sound may be normal in children and in pregnancy. Similarly, an S4 may be commonly heard in the elderly.
When S3 or S4 is associated with tachycardia, it is called a gallop rhythm either S3 or S4 gallop. S3 gallop is also known as protodiastolic gallop. S4 gallop is otherwise known as presystolic gallop.
In tachycardia, S3 may fuse with S4 and produce a summation gallop.
First heart sound: First heart sound is a high pitched sound and is heard best with the diaphragm of the stethoscope. It is best heard at the cardiac apex. First heart sound is timed in relation to the carotid pulse as it occurs at the onset of systole. Interval between the first and second heart sounds constitutes the clinical systole and that from second heart sound to the next S1 the clinical diastole.
A loud S1 is heard in mitral stenosis while a soft S1 is heard in mitral regurgitation. Intensity of S1 decreases with decreasing left ventricular systolic function. In severe calcific mitral stenosis, when the valve becomes very stiff, intensity of S1 may decrease. Intensity of S1 increases in tachycardia when the diastolic period is shortened.
Split of S1 is not audible usually but may be heard in right bundle branch block and Ebstein’s anomaly of the tricuspid valve. In the latter condition, the loud tricuspid component, that is T1, is known as sail sound and it is due to the closure of the large anterior tricuspid leaflet.
Second heart sound is also a high pitched sound, better heard with the diaphragm of the stethoscope. Aortic component or A2 is loud in systemic hypertension and soft in aortic stenosis. P2 is loud in pulmonary hypertension and soft in pulmonary stenosis.
Wide fixed split of S2 is a feature of atrial septal defect. Wide variable split may be heard in right bundle branch block due to delayed closure of the pulmonary valve. Paradoxical split can occur in left bundle branch block and aortic stenosis. But it is often difficult to appreciate in the latter condition due to the preceding loud murmur.
Third heart sound is a low pitched sound and hence better heard with the bell of the stethoscope. Left ventricular S3 is usually a feature of left ventricular failure and best heard at the apex. S3 in mitral regurgitation need not imply left ventricular failure while an S3 in aortic regurgitation implies left ventricular failure. A right ventricular S3 may be heard medial to the apex beat in the tricuspid area in right ventricular failure.
Fourth heart sound occurs when there is a forceful atrial contraction and is common in the elderly with a stiff left ventricle. S4 is designated as an atrial sound, though it possibly originates in the ventricle. It can occur in acute ischemia of the myocardium when the relaxation of the left ventricle is impaired. Being a low pitched sound, it is better heard with the bell of the stethoscope.
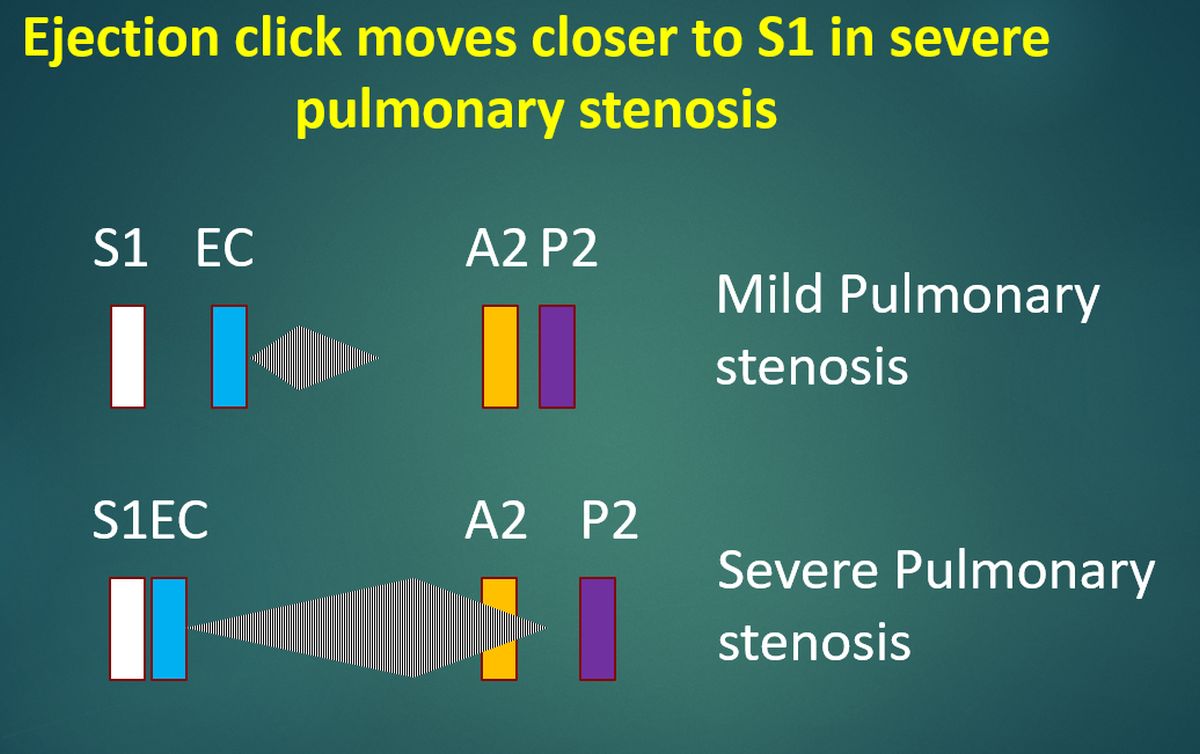
Clicks may be divided into ejection and non-ejection clicks. The click of mitral valve prolapse is a non-ejection click. It is typically mid systolic. Ejection clicks are heard in aortic and pulmonary stenosis. Vascular ejection clicks may be heard when the aorta or pulmonary artery is dilated.
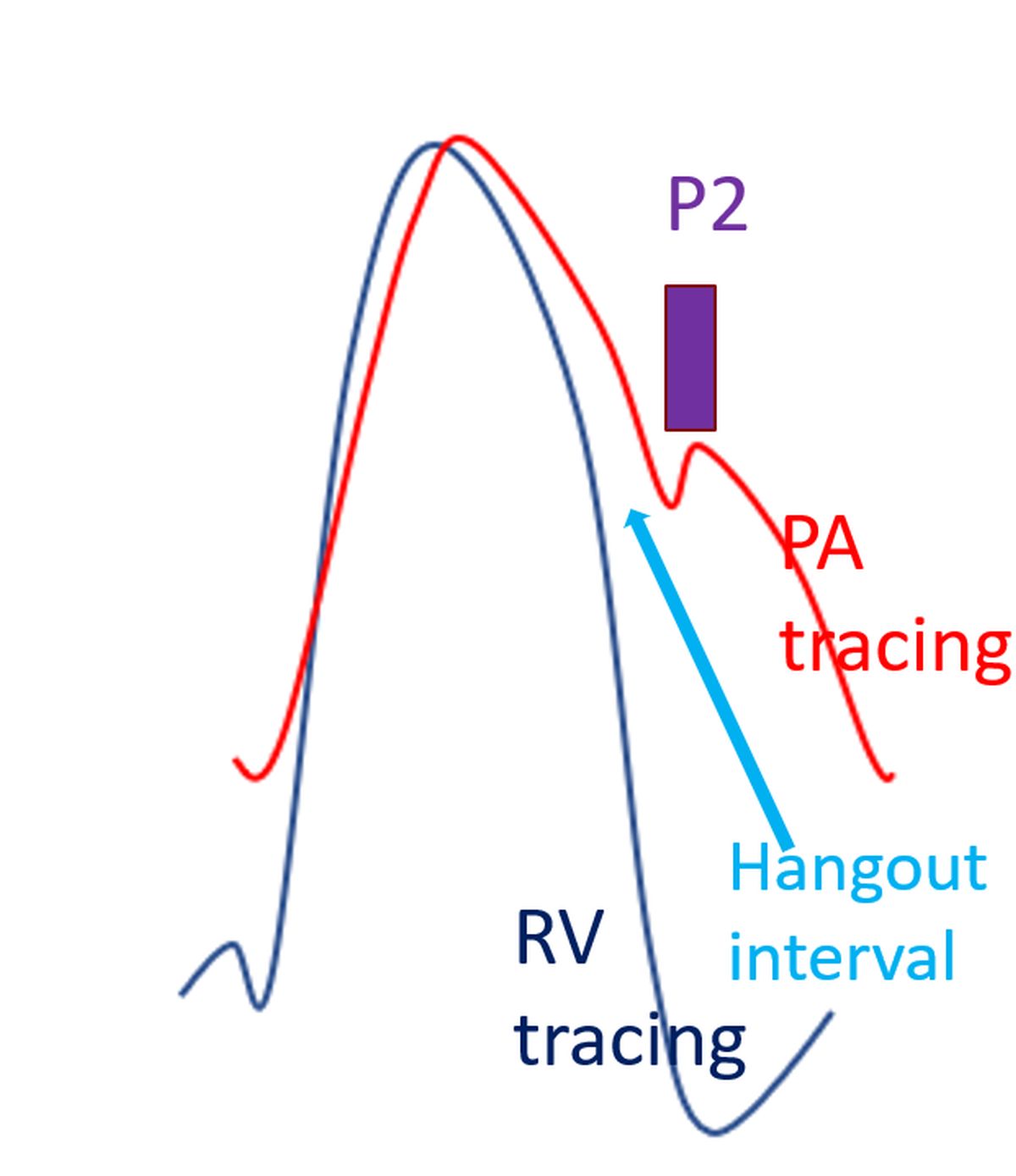
Pulmonary ejection clicks become closer to the first heart sound as the severity of pulmonary stenosis increases. It is the only right sided event which becomes more prominent in expiration.
The phasic nature is due to changes in the pulmonary hang out interval. Hang out interval is the time delay for closure of the pulmonary valve after the crossover of the pulmonary and right ventricular pressure tracings. Longer hang out interval of the pulmonary valve than the aortic valve is due to the lower resistance of the pulmonary circulation.
A phasic aortic ejection click may be heard in tetralogy of Fallot. It is a vascular ejection click due to the dilated aorta which receives blood from both ventricles.
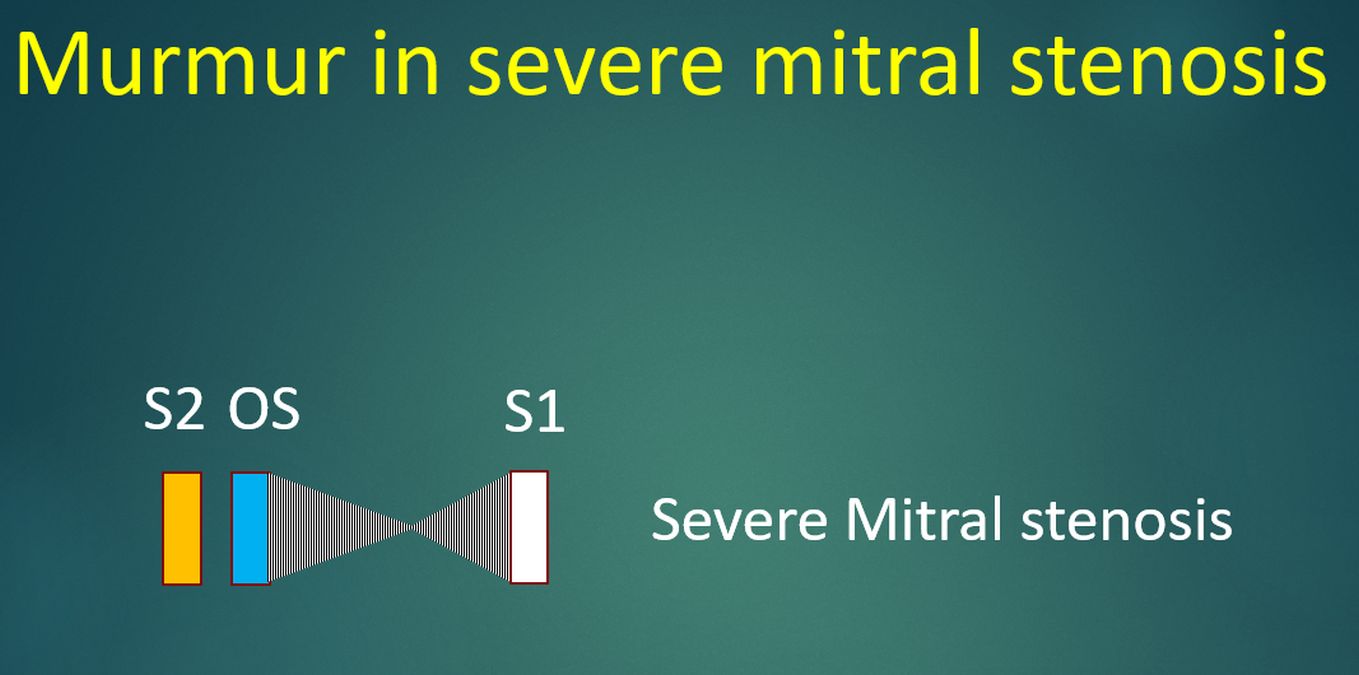
Opening snap is typically heard in mitral stenosis, though it may be there in tricuspid stenosis, it is seldom appreciated in tricuspid stenosis. Opening snap is a sharp, high pitched sound, heard better with the diaphragm of the stethoscope. It is heard best slightly medial to the apex rather than the at the apex.
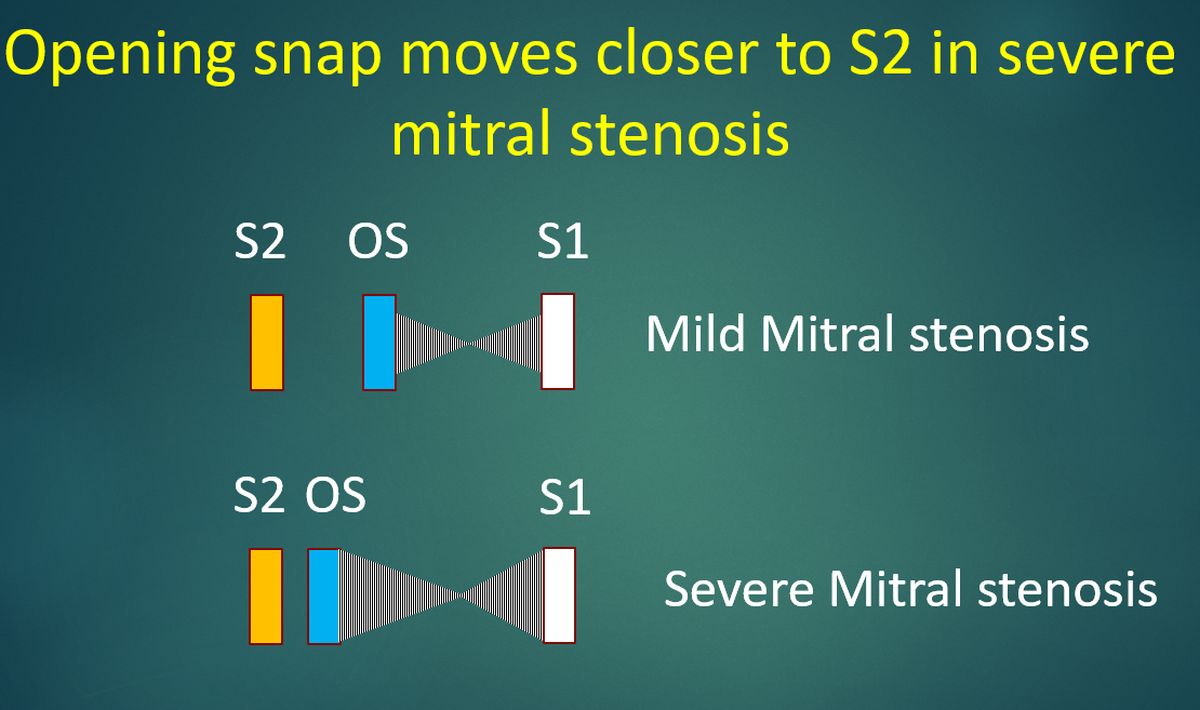
Opening snap occurs after the second heart sound and is earlier in severe mitral stenosis. Hence S2-OS interval is inversely related to severity of mitral stenosis. Opening snap disappears when the valve becomes non pliable with severe calcification. The mid diastolic murmur of mitral stenosis starts immediately after the opening snap.
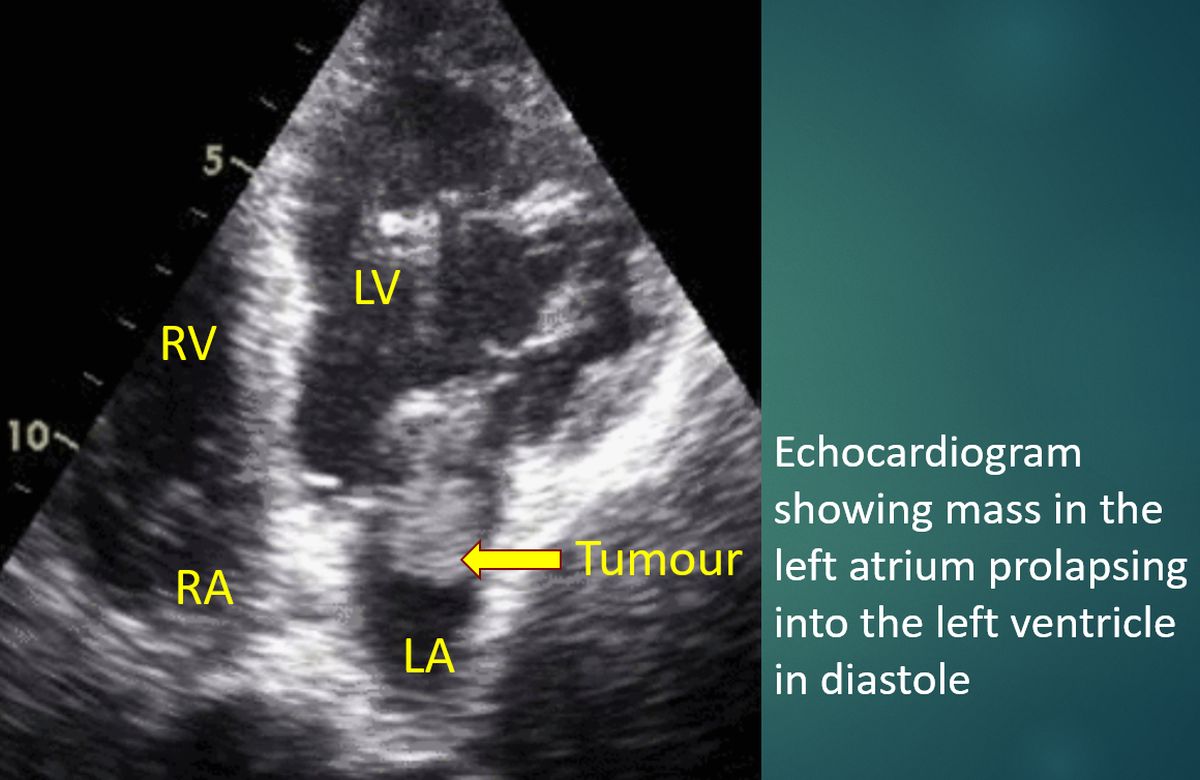
Tumor plop occurs soon after the second sound when a pedunculated atrial myxoma (right or left) pops into the tricuspid or mitral orifice in early diastole. It occurs when the diastolic movement of a tumor with a large stalk into the ventricle is abruptly stopped.
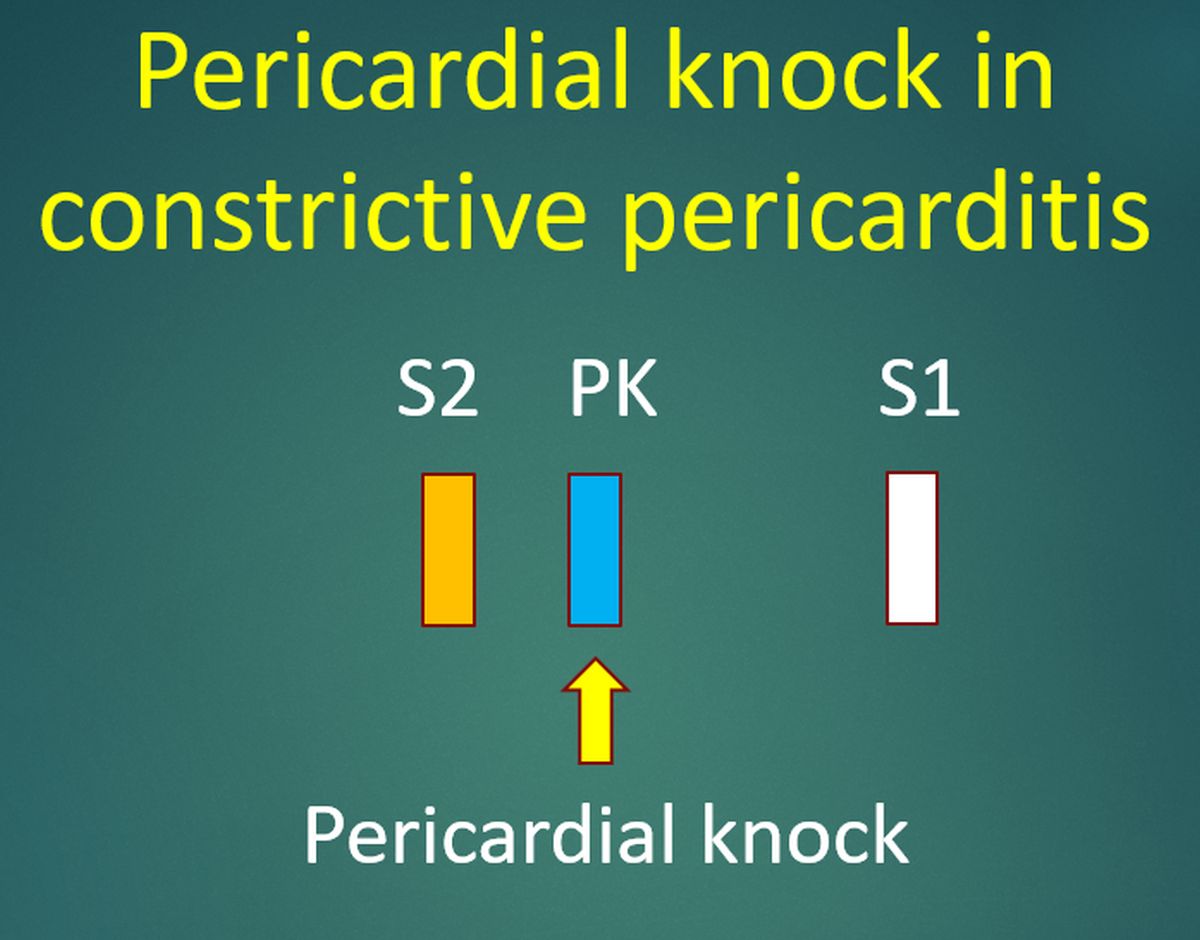
Pericardial knock is an early diastolic sound heard in constrictive pericarditis. It is also called and ‘early S3’. The sudden rush of blood flow from the atria to the ventricles is halted soon by the thickened pericardium which causes restraint for ventricular relaxation, leading to pericardial knock.
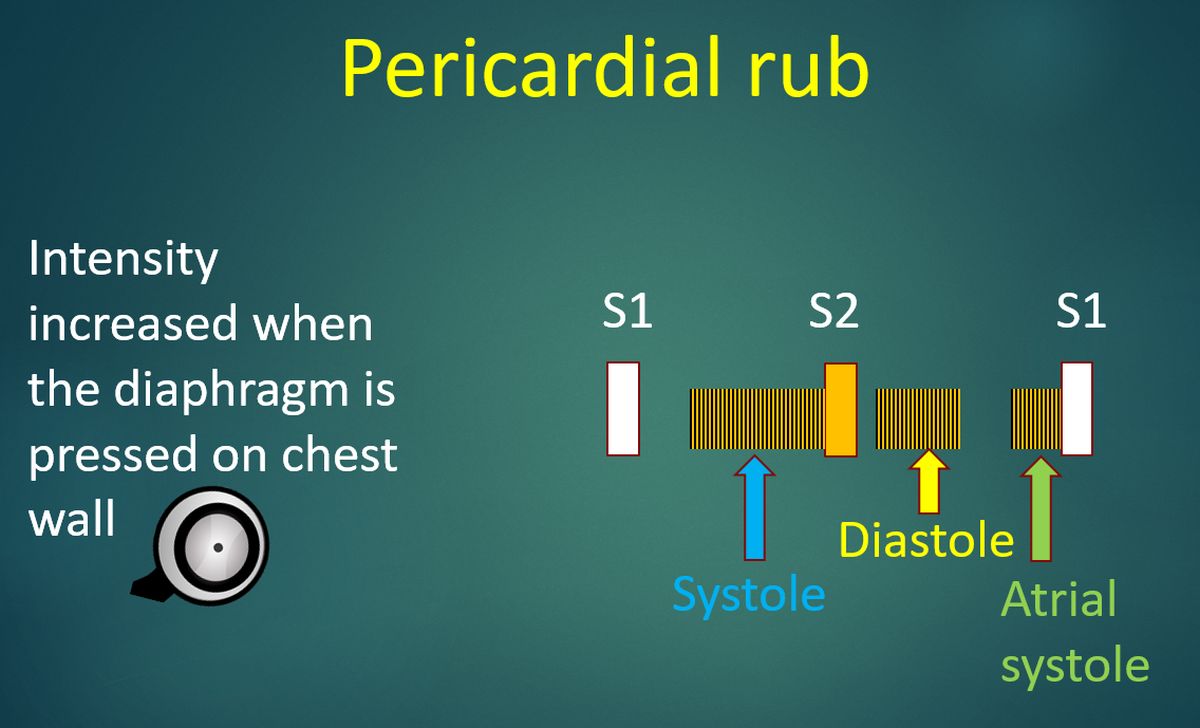
Pericardial rub is a superficial scratchy sound which is better heard with the person leaning forward. Intensity increases when the diaphragm is pressed on the chest wall. It persists on breath holding and is synchronous with the heart beats, differentiating it from the pleural rub. Pericardial rub is triphasic, with one phase each in systole, diastole and atrial systole. All phases may not be heard always and it is well known to be evanescent.
Now we move on to cardiac murmurs.
Cardiac murmurs are initially classified into systolic, diastolic and continuous.
They can be timed in relation to the carotid pulse.
A systolic murmur starts with or after the first heart sound and ends at or before the second heart sound. Clinically, systole can be timed with the onset of carotid pulse.
Diastolic murmurs start with or after the second heart sound.
By definition, a continuous murmur starts in systole, persists through the second heart sound, into the diastole.
When the pressure gradient is high between the two chambers across which the murmur is generated, the murmur is high pitched.
Levine’s grading of murmurs
The initial grading was based on the intensity of the murmur alone.
Later presence of thrill was added, with thrill being appreciated in murmurs of grade IV and above.
Conventionally, grading is considered for systolic murmurs.
1. Grade I: Faint murmur audible only on auscultation in a quiet room by an expert.
2. Grade 2: Slight murmur
3. Grade 3: Moderate intensity murmur
4. Grade 4: Loud murmur
5. Grade 5: Very loud murmur
6. Grade 6: Loudest murmur. It is mentioned that grade 6 murmurs are audible with the stethoscope close to the chest without actual contact.
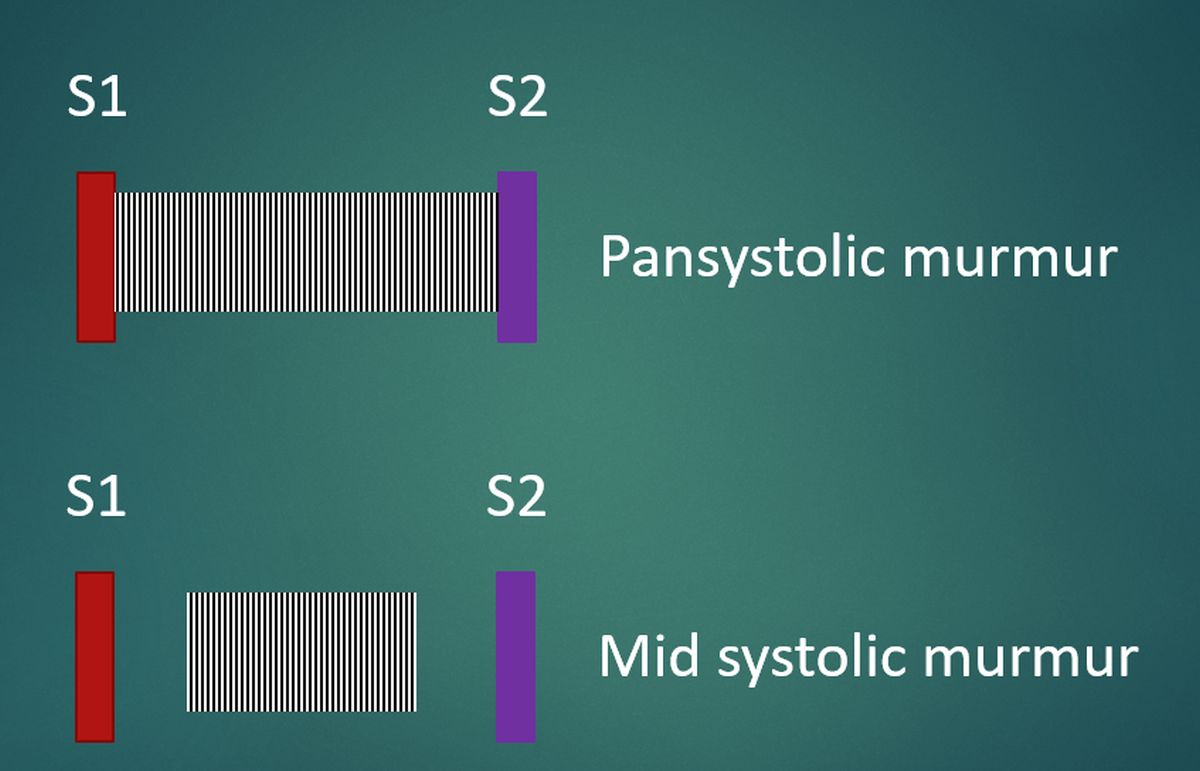
A murmur which extends throughout the systole is called pansystolic murmur (Also known as holosystolic murmur). Important pansystolic murmurs are those due mitral and tricuspid regurgitation and that of a ventricular septal defect.
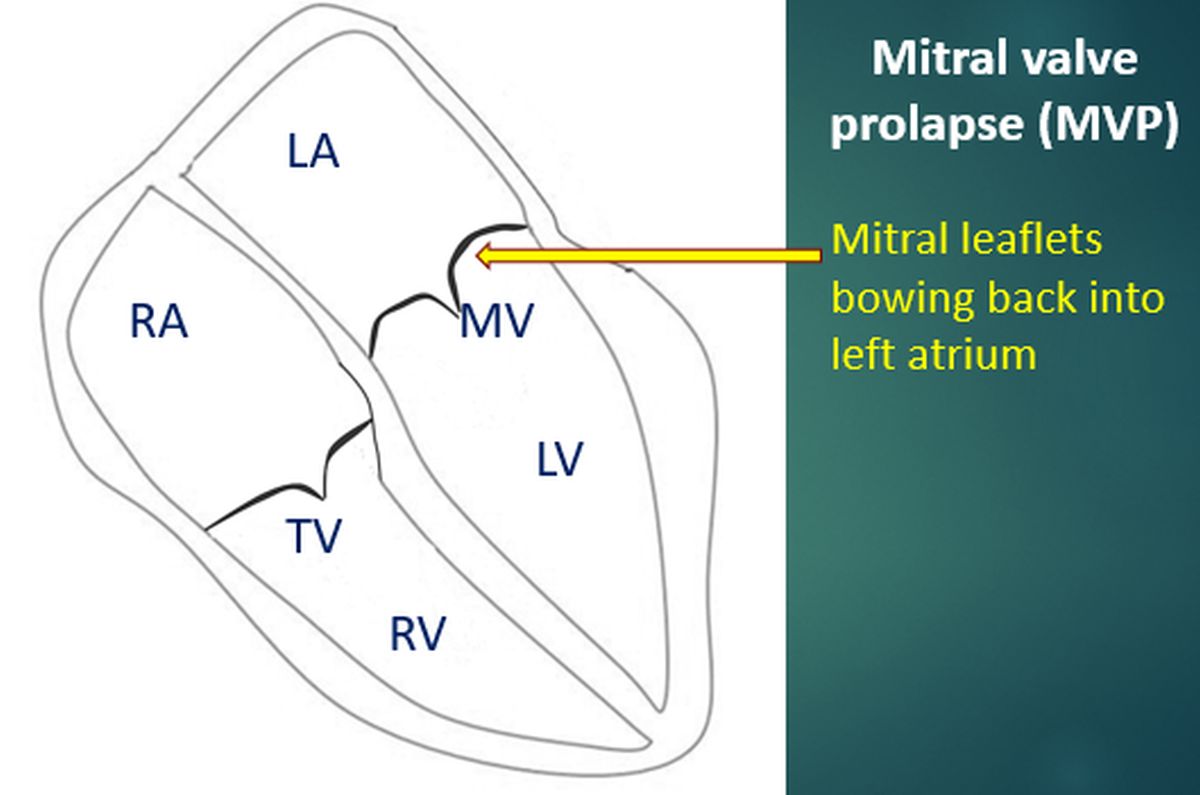
Mid systolic murmur starts a short period after the onset of systole. Typical mid systolic murmur is that of mitral valve prolapse.
Late systolic murmur could also be there in mitral valve prolapse.
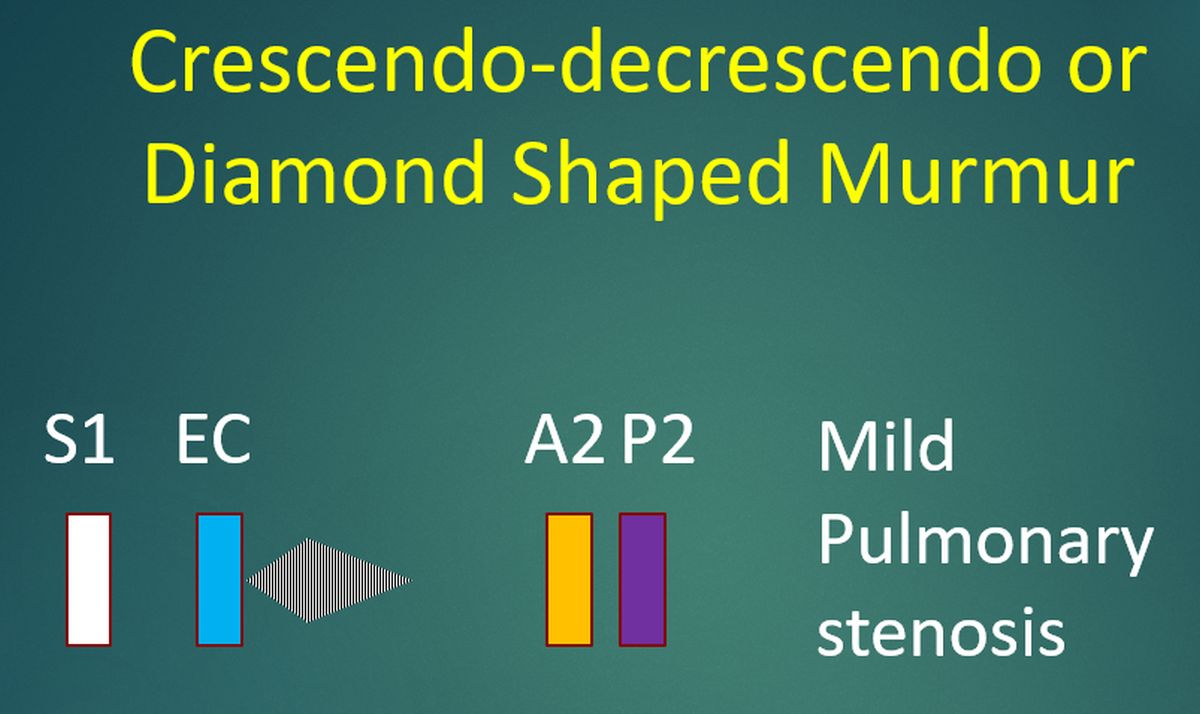
Ejection systolic murmurs of pulmonary and aortic stenosis start a short while after the onset of systole (S1) and is preceded by the ejection click.
They are crescendo-decrescendo murmurs or diamond shaped murmurs.
The length of these murmurs are directly related to the severity of stenosis.
In ventricular septal defect, a loud murmur usually indicates a small defect with large pressure gradient across the defect.
In large ventricular septal defect, due to the large left to right shunt, pressure in the right ventricle increases (hyperdynamic pulmonary hypertension) so that pressure in the two ventricles are nearly equal.
This results in a soft murmur.
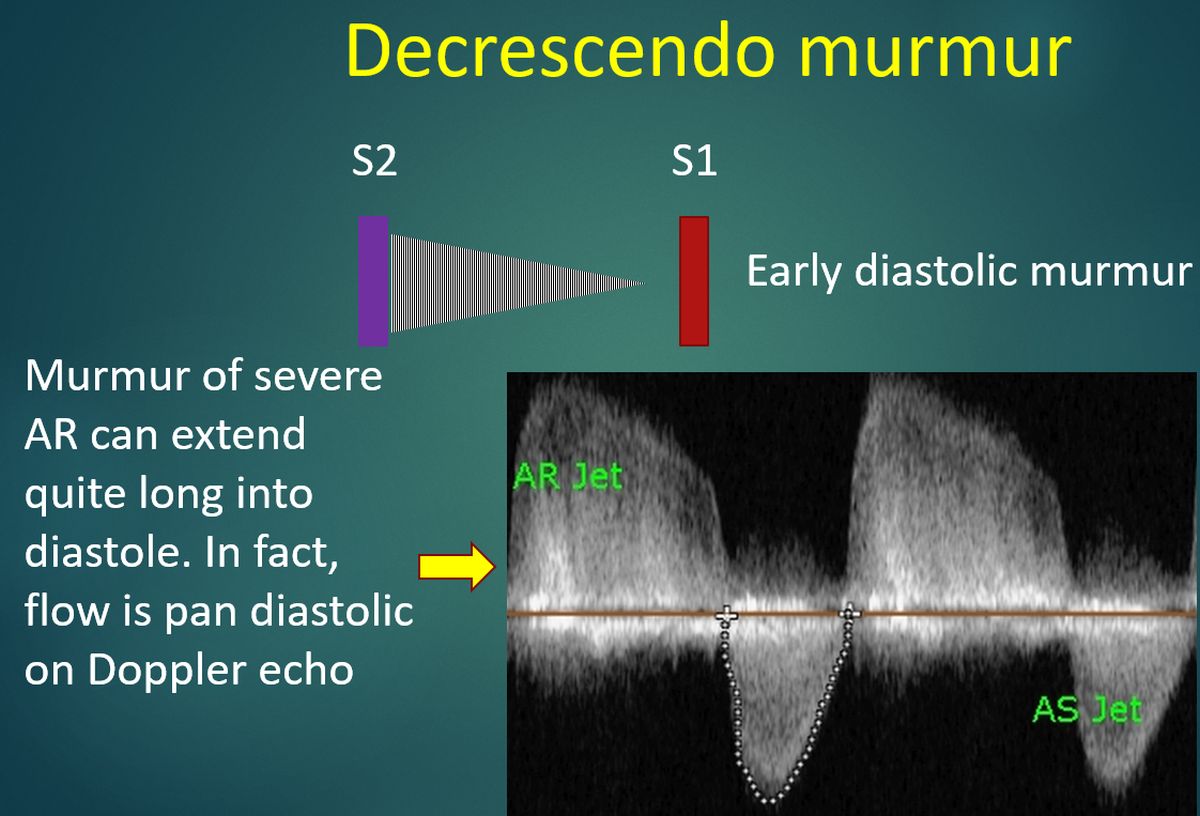
Early diastolic murmur starts with the second heart sound.
Typical early diastolic murmurs are those of aortic regurgitation and pulmonary regurgitation due to pulmonary hypertension (Graham steel murmur).
They are decrescendo murmurs.
In pulmonary regurgitation without pulmonary hypertension, the murmur starts a short while after the second heart sound (delayed diastolic murmur).
In mitral and tricuspid stenosis, there is a mid-diastolic murmur.
The mitral diastolic murmur heard in severe aortic regurgitation (Austin Flint murmur) could be either mid diastolic or late diastolic murmur (pre-systolic murmur).
Continuous murmurs start in systole and continue through the second heart sound into a variable part of the diastole.
Some of these murmurs are heard throughout the cardiac cycle.
The classical continuous murmur is that of patent ductus arteriosus (Gibson’s murmur).
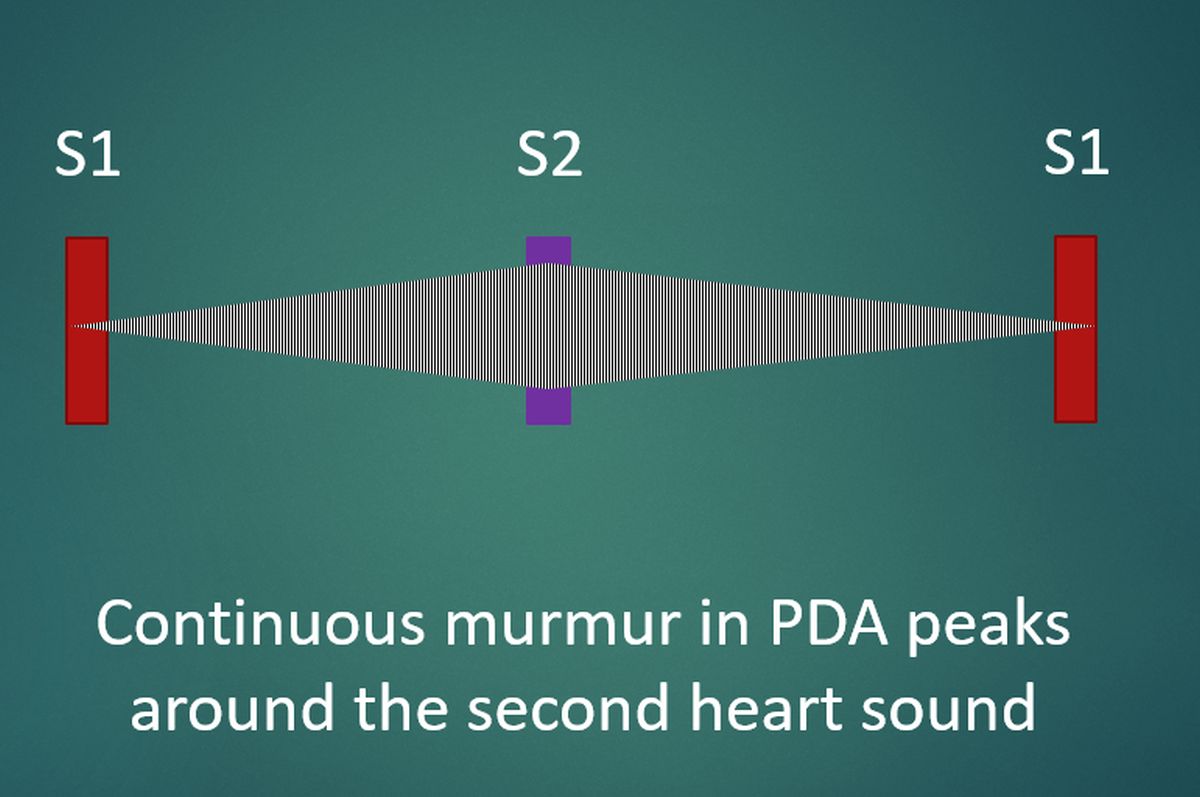
The region where this murmur is best heard below the left clavicle is known as Gibson’s area.
The murmur of patent ductus arteriosus peaks over the second heart sound.
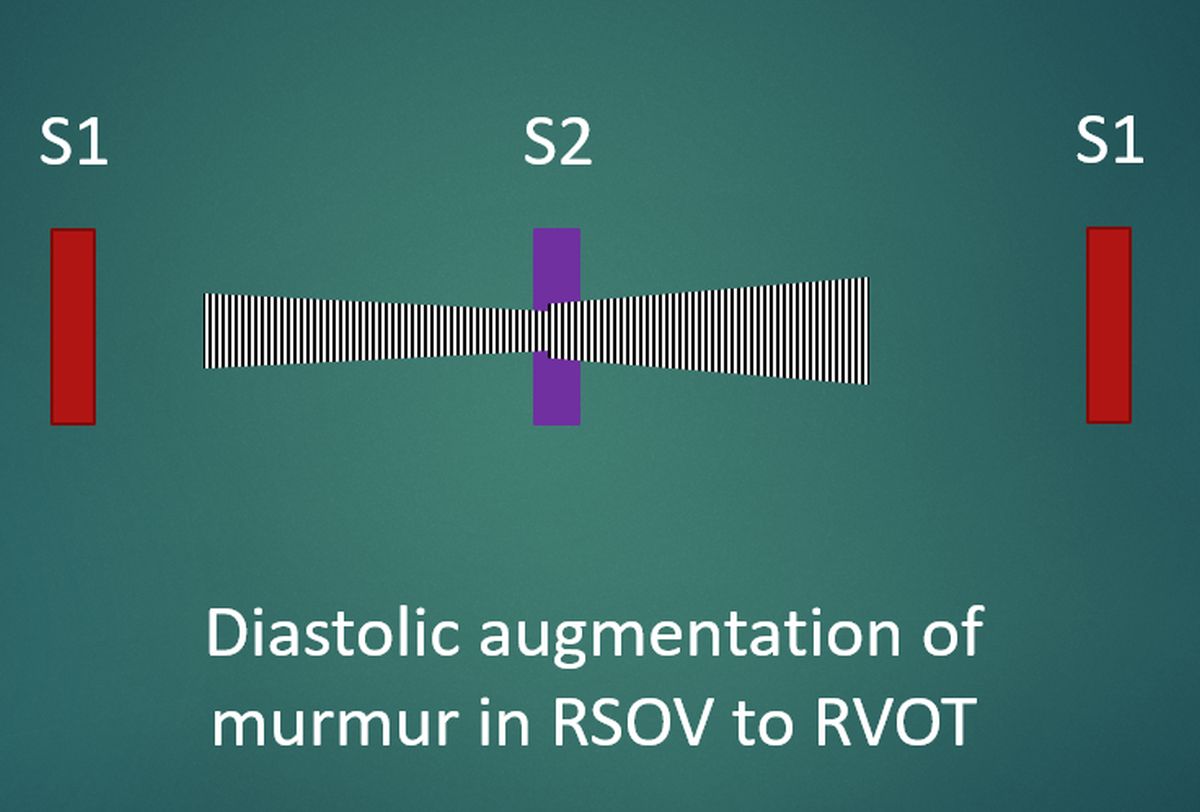
Another cause of continuous murmur is the rupture of sinus of Valsalva into the right atrium or right ventricle.
The continuous murmur of rupture of sinus of Valsalva into right ventricle typically produces a murmur which peaks in diastole.
This is because the track which passed through the right ventricular muscle gets compressed during systole, reducing the intensity of the murmur in systole.