ECG in coronary artery disease
ECG in coronary artery disease
ECG changes in coronary artery disease (CAD) can be in any of the waves or segments. Diagnosis of acute myocardial infarction in the emergency room still relies mostly on the ECG, though other investigations are there to supplement.
P wave abnormalities
P wave abnormalities have been described as minor ECG criteria of atrial infarction [1]. Abnormal P waves described are M-shaped, W-shaped, irregular or notched. There can be evidence of left atrial enlargement if there is left ventricular dysfunction. Atrial arrhythmias can be observed in atrial infarction.
Abnormalities of PR segment
PR segment contains the atrial repolarization wave (Ta) though it is not usually evident. PR segment depression can occur in atrial infarction. An old article discusses abnormalities of P-Ta segment as major ECG criteria for the diagnosis of atrial infarction [1]. These criteria are: elevation of P-Ta segment of over 0.5 mm in V5, V6 with reciprocal depression in V1, V2; elevation of P-Ta segment of over 0.5 mm in lead I and depression in leads II or III; depression of P-Ta segment of more than 1.5 mm in precordial leads and 1.2 mm in leads I, II, and III in the presence of any form of atrial arrhythmia. P-Ta segment was later called PQ segment [2] and now as PR segment. PQ segment depression can occur in pericarditis associated with acute Q wave inferior wall myocardial infarction as per a study [2]. That study also diagnosed 5 cases of atrial infarction among their 171 patients, based on ECG criteria. Two of these patients had PQ segment elevation in I and aVL. Other 3 were suspected based on P wave abnormalities.
QRS abnormalities
Pathological Q waves are noted in old myocardial infarction (necrosis of myocardium due loss of blood supply). Following features are important in recognizing a pathological Q wave:
- Width of 1 mm (40 ms or 0.04 s) or more.
- Depth of 25% or more of the ensuing R wave.
It may be noted that width is more important than depth in recognizing a pathological Q wave. All Q waves are not due to old infarction. Q waves may be seen in hypertrophic cardiomyopathy and muscular dystrophy.
Loss of R wave progression in anterior leads is a commonly sought feature of old anterior wall myocardial infarction. But it may be noted that this can also occur in emphysema. Normally the amplitude of R waves increase from V1 to V5 or V6, while S waves decrease in amplitude.
ST segment abnormalities
ST segment abnormalities are common in the acute stage of myocardial ischemia and infarction. It is usually mentioned that subendocardial ischemia produces ST depression while transmural ischemia produces ST elevation. ST elevation is an important feature of ST elevation myocardial infarction (STEMI). ST elevation which is upsloping in the hyperacute phase of myocardial infarction becomes convex (coved) in the evolving phase when the T wave gets inverted. ST elevation in hyperacute phase of myocardial infarction is known as Pardee’s sign [3,4]. ST depression in acute ischemia may be upsloping, horizontal or down sloping. Of these, upsloping ST depression is least specific and can occur as a normal variant. Down sloping ST depression is also seen in ventricular hypertrophy with strain pattern including hypertrophic cardiomyopathy.
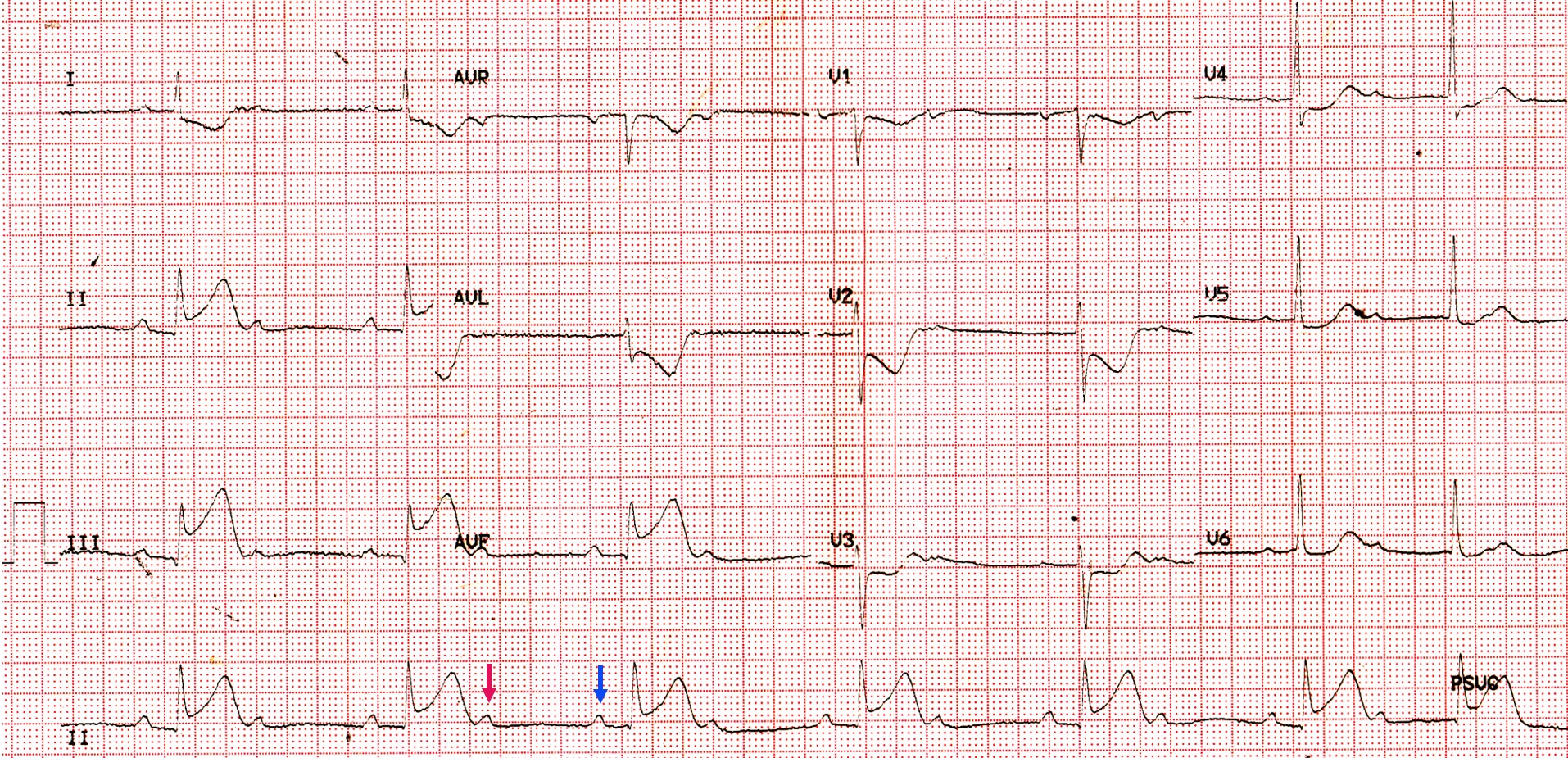
T wave abnormalities
T wave abnormalities are common in myocardial ischemia and infarction, but lack specificity. T inversions in anterior leads can occur as a normal variant in younger individuals (juvenile pattern or juvenile T inversion). Ischemic T inversion is usually symmetric and arrow head like while that due to hypertrophy strain pattern is asymmetric. Tall T waves with upsloping ST segment may be seen in hyperacute phase of myocardial infarction, though it can sometimes be a normal variant. When in doubt, repeating ECG after a short period of observation to look for serial evolution or supplementary investigations like echocardiography are useful. This is mandatory when the clinical history is in favor of myocardial ischemic pain.
Conduction abnormalities
Conduction abnormalities are not uncommon in myocardial infarction as it can affect the blood supply of the conduction system including bundle of His and its branches. SA nodal and AV nodal conduction abnormalities including complete heart block can occur in inferior wall myocardial infarction due to occlusion of right coronary artery. Though new onset left bundle branch block was considered as a surrogate of acute myocardial infarction earlier, it is no longer so. Left anterior hemiblock is the commonest conduction abnormality in anterior wall myocardial infarction and has no prognostic significance. Right bundle branch block in association with anterior wall myocardial infarction carries a poorer prognosis because of more extensive myocardial damage. Presence of associated left posterior hemiblock implies a still worse prognosis. This is because of dual blood supply of posterior fascicle. Complete heart block along with anterior wall myocardial infarction signifies very extensive myocardial infarction and has the worst prognosis.
Arrhythmias
Ventricular ectopic beats are the most common arrhythmia seen in the acute phase of myocardial infarction due to irritability of the myocardium. They progress to ventricular tachycardia and fibrillation sometimes. Ventricular fibrillation occurring during the first 24 hours of infarction is often primary ventricular fibrillation. Secondary ventricular fibrillation is that which occurs after the onset of cardiac failure and is not so well treatable as primary ventricular fibrillation which occurs in the early phase of acute myocardial infarction. Another type of ventricular fibrillation in the setting of acute myocardial infarction is late in hospital ventricular fibrillation. Atrial ectopic beats indicate left atrial dilatation consequent to left ventricular dysfunction. Coronary intensive care units were initially designed to pick up arrhythmias early and treat them, improving the prognosis in the acute phase.
References
- Liu CK, Greenspan G, Piccirillo RT. Atrial infarction of the heart. Circulation. 1961 Mar;23:331-8.
- Nagahama Y, Sugiura T, Takehana K, Tarumi N, Iwasaka T, Inada M. PQ segment depression in acute Q wave inferior wall myocardial infarction. Circulation. 1995 Feb 1;91(3):641-4.
- Pardee HEB. An electrocardiographic sign of coronary artery obstruction. Arch Intern Med 1920; 26: 244– 257.
- de Bliek EC. ST elevation: Differential diagnosis and caveats. A comprehensive review to help distinguish ST elevation myocardial infarction from nonischemic etiologies of ST elevation. Turk J Emerg Med. 2018 Feb 17;18(1):1-10.