ECG monitoring in ICU
ECG monitoring in ICU
Goals of ECG monitoring
Following are the usual goals of ECG monitoring in the intensive coronary care unit:
- Heart rate and basic rhythm determination
- Diagnosis of complex arrhythmias
- Detection of ischemia and prolonged QT interval
Advanced monitoring facilities may be used for the following features which are yet to be well established:
- Computerized ST segment analysis
- Computerized arrhythmia analysis
- Computerized QT-interval monitoring
Improvements in ECG monitoring
Over the past few decades since the initiation of ECG monitoring in the 1960s, several improvements have occured. They include improved noise reduction strategies, multilead monitoring and derived 12-lead ECGs.
Cardiac arrhythmia monitoring
Cardiac arrhythmia monitoring is needed for all patients at significant risk of an immediate, life-threatening arrhythmia, which include: Post cardiac arrest, early phase of acute coronary syndrome, post cardiac surgery and after anesthesia. Battery-operated monitor-defibrillators are useful while transporting such patients. Personnel watching the monitor in the ICU should have skill in ECG interpretation and defibrillation.
ST-segment ischemia monitoring
In the setting of an acute myocardial infarction ST segment ischemia monitoring is useful to assess the patency of culprit artery after thrombolysis, abrupt reocclusion after primary angioplasty and to detect ongoing ischemia / infarct extension. ST segment monitoring is not useful in left bundle branch block, ventricular paced rhythm, arrhythmias that obscure the ST Segment and in patients who are agitated.
Improving the quality of ST-segment ischemia monitoring
Following steps are useful in improving the quality of ischemia monitoring: ST-segment should be evaluated only in supine position. Careful skin preparation should be done to improve the lead contact. Consistent lead placement is needed for comparisons. Ideally the electrode positions have to be marked with a skin marking pencil. ST alarm parameters have to be set based on the patient’s baseline ST Level.
QT interval monitoring for detection of proarrhythmia
QT interval monitoring is useful in patients on anti arrhythmic drugs known to cause torsades de pointes (TDP). It is also useful in the overdose of a potentially proarrhythmic agents, patients with new-onset bradyarrhythmias and in those with severe hypokalemia or hypomagnesemia.
Electrode positioning for cardiac monitoring
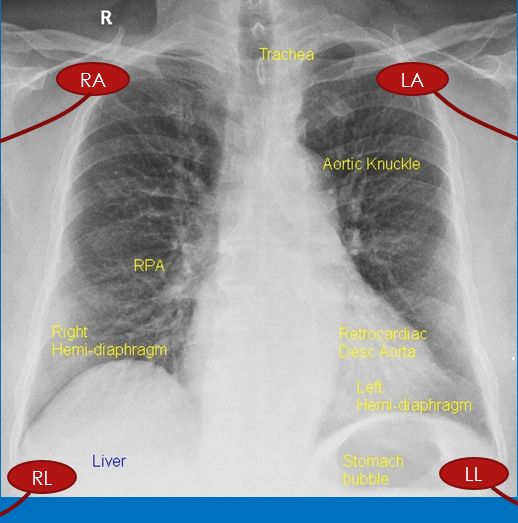
Limb electrodes are placed on torso to reduce muscle artifact during limb movement and also to avoid tethering of the patient. Right arm/left arm leads are placed in the corresponding infraclavicular fossa. Left leg electrode is placed below the rib cage on the left side of abdomen. Right leg electrode can be placed anywhere on the right side the abdomen.
Which lead to monitor?
Have a look at the 12 lead ECG before deciding on which lead to monitor. Usually lead II is monitored in most patients as it gives good P waves for rhythm interpretation. But in several patients, limb lead voltages may be low so that heart rate counting becomes erroneous. Good R wave amplitude is needed for counting the heart rate accurately so that false alarms can be avoided. If T wave is very tall in the monitoring lead, it leads to T wave oversensing and dual counting sometimes. When limb leads do not give P and QRS complexes, chest lead monitoring may be needed in some cases. Usually ICU staff prefer not to use chest lead monitoring as it interferes with auscultation, echocardiography and even defibrillation in case of an emergency.
How to monitor chest leads in an simple monitor with only three electrode cables?
Some monitors, especially defibrillator-monitors have only three cables. Two of them are active and one is a ground electrode. These are usually used as modified limb lead monitors, typically in lead II configuration with leads attached to the torso near the limb. Modified chest leads MCL1 to MCL6 configurations can be used to monitor chest leads with two electrode cables. For MCL1, the negative pole is kept in the left infraclavicular fossa and positive pole in the fourth right intercostal space close to sternum (V1 position). For other MCL leads, the positive pole is shifted to the corresponding chest lead positions.
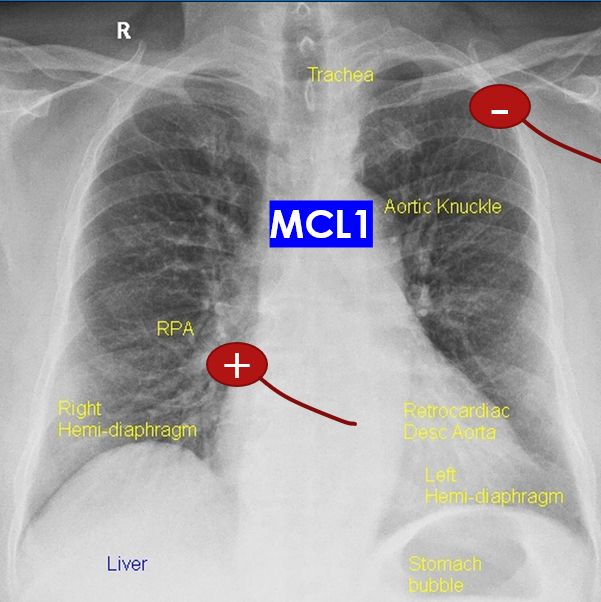
The combination for lead I can be used in reverse manner for MCL. Right arm electrode is kept in left infraclavicular fossa and left arm electrode in V1 position. Unlike the usual chest leads which are unipolar MCL1 is bipolar. If electrodes for lead II are being used, left arm electrode can be placed in left infraclavicular fossa and left leg electrode in V1 position. Using multiple limb leads is possible only in monitors with 4 electrode cables (three active + one ground).
Reference
- Drew BJ, Scheinman MM. Value of electrocardiographic leads MCL1, MCL6 and other selected leads in the diagnosis of wide QRS complex tachycardia. J Am Coll Cardiol. 1991 Oct;18(4):1025-33.


