Extracorporeal CPR (ECPR)
Extracorporeal CPR (ECPR)
Conventional cardiopulmonary resuscitation (CPR) involves chest compressions and respiratory support with either mouth to mouth respiration or bag and mask ventilation. Extracorporeal CPR (ECPR) means supporting the heart and lung function using extracorporeal method of venoarterial perfusion during cardiac arrest [1]. Extracorporeal membrane oxygenator (ECMO) circuits are used in extracorporeal CPR.
2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care [2] discusses the use of ECPR for cardiac arrest and also the potential ethical issues. Ethical issues arise as the decision to discontinue CPR in this situation becomes more complicated. ECPR may be considered in cases of refractory cardiac arrest when the cause of the cardiac arrest is likely to be reversible.
2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care [3] mentions two knowledge gaps on extracorporeal CPR. They are (1) Which populations are most likely to benefit from extracorporeal CPR? (2) What is the role of extracorporeal CPR for infants and children with out-of-hospital cardiac arrest and in-hospital cardiac arrest due to noncardiac causes?
No randomized controlled trials on ECPR have been published so far, though observational studies are available [4]. ECPR is implemented when there is no prompt return of spontaneous circulation (ROSC) with conventional CPR.
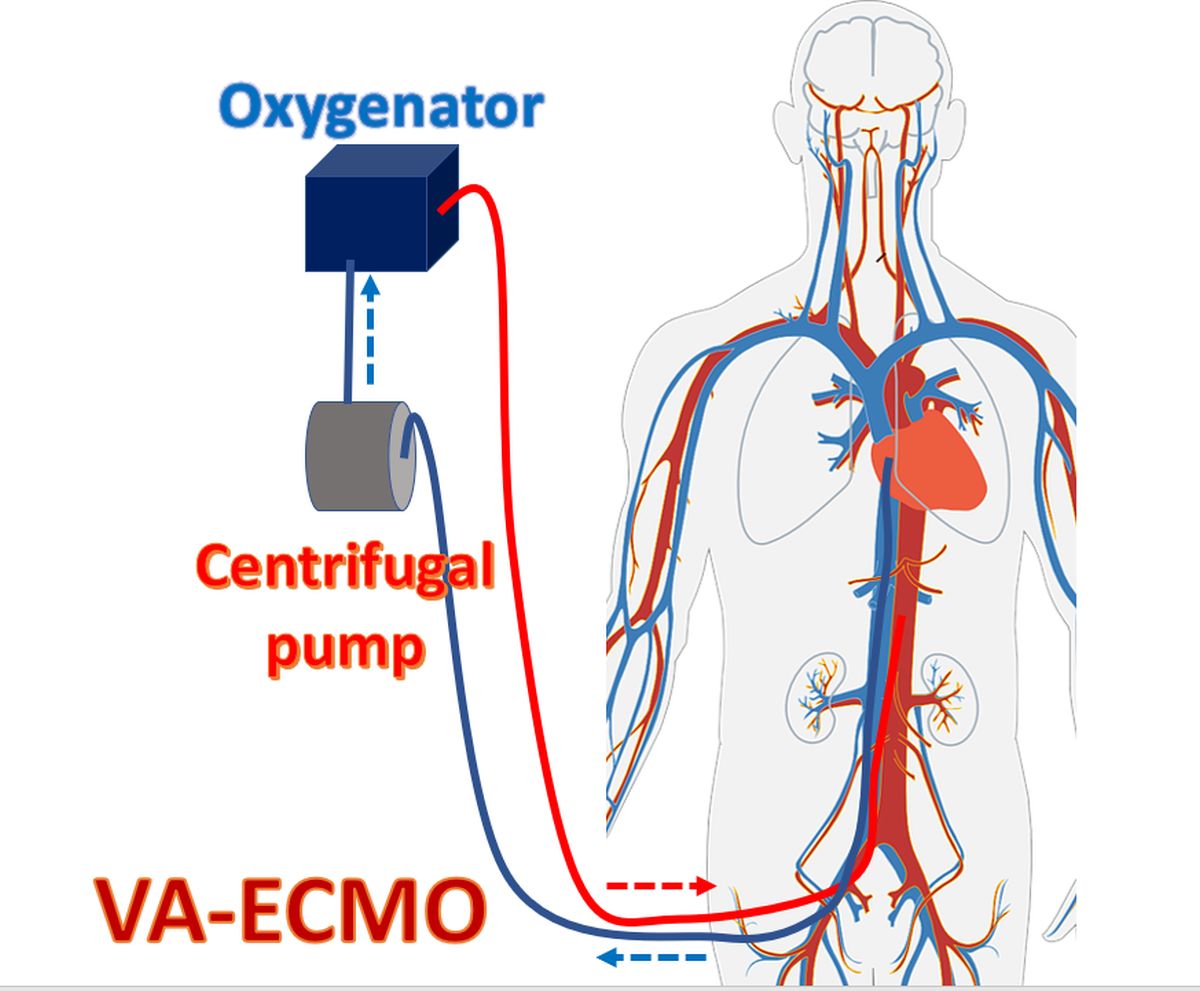
In venoarterial ECMO, the venous blood is removed from a catheter placed in the right atrium through the femoral vein. The blood oxygenated by the ECMO device is returned through a catheter introduced via the femoral artery to the distal aorta. ECMO device differs from the conventional heart lung machine setup in that it is portable to be applied at the bedside and the catheters are introduced percutaneously or by vessel cut down instead of being introduced after thoracotomy.
In the CHEER trial (mechanical CPR, Hypothermia, ECMO and Early Reperfusion) [4] extracorporeal CPR could be established in 24 of the 26 eligible patients, with a median time of 56 minutes from the onset of collapse. Survival to hospital discharge with full neurological recovery occurred in 14 of them. 11 of 26 eligible patients had out-of-hospital cardiac arrest while 15 had in-hospital cardiac arrest. Hypothermia was induced by intravenous administration of ice-cold saline as per their protocol. Percutaneous cannulation of the femoral artery and vein were done by two critical physicians for commencement of venoarterial ECMO. Those with suspected coronary artery occlusion were transferred for coronary angiography. Therapeutic hypothermia was maintained for 24 hours in the intensive care unit.
While conventional CPR provides only about a quarter of the normal cardiac output, ECPR can provide sufficient perfusion to vital organs and reduce the duration of low flow status [5]. Rapid achievement and maintenance of targeted temperature management is possible with ECPR because of the availability of heat exchanger. Another advantage cited for ECPR is the facilitation of coronary interventions even in patients with sustained ventricular fibrillation because VA-ECMO provides stable systemic perfusion [5].
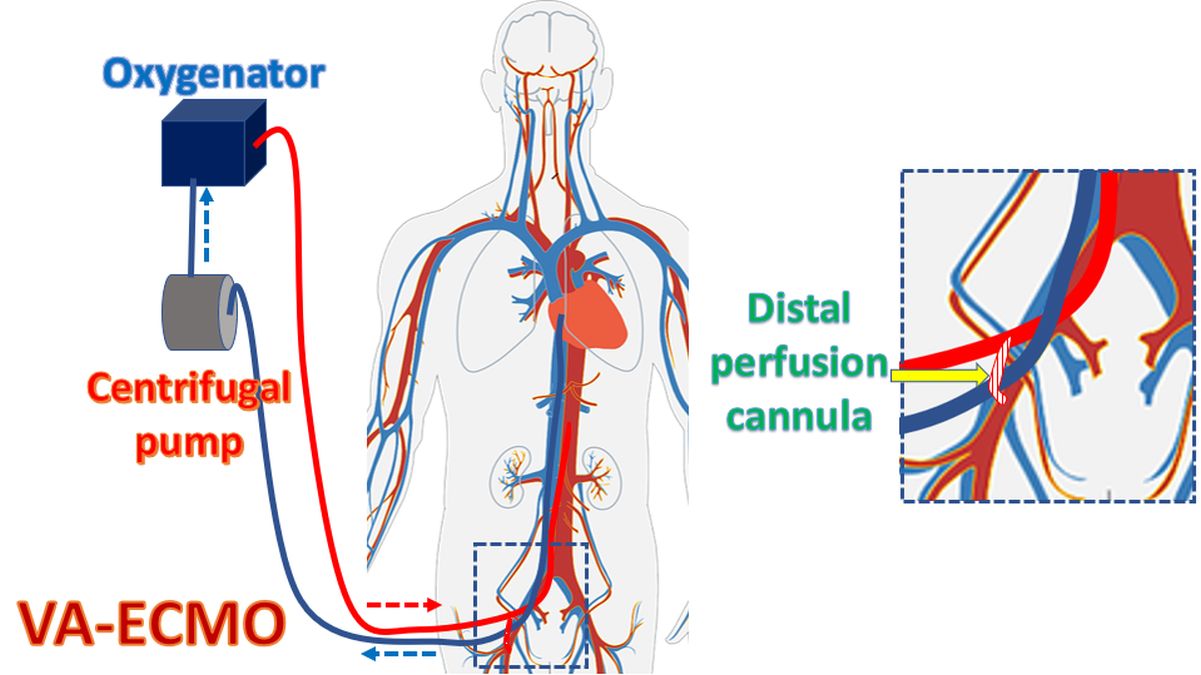
Bleeding, limb ischemia and sepsis are the important complications of extracorporeal CPR. Limb ischemia is taken care of by a distal perfusion cannula to improve distal flow in the femoral artery. The distal perfusion cannula connects the arterial return line from the oxygenator to the distal femoral artery, so that a portion of the oxygenated blood is used to perfuse the distal lower limb beyond the point of connection of the main femoral arterial ECMO line.
References
-
- Younger JG, Schreiner RJ, Swaniker F, Hirschl RB, Chapman RA, Bartlett RH. Extracorporeal resuscitation of cardiac arrest. Acad Emerg Med. 1999 Jul;6(7):700-7.
- Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, Brooks SC, de Caen AR, Donnino MW, Ferrer JM, Kleinman ME, Kronick SL, Lavonas EJ, Link MS, Mancini ME, Morrison LJ, O’Connor RE, Samson RA, Schexnayder SM, Singletary EM, Sinz EH, Travers AH, Wyckoff MH, Hazinski MF. Part 1: Executive Summary 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015; 132: S315-S367.
- Merchant RM, Topjian AA, Panchal AR, Cheng A, Aziz K, Berg KM, Lavonas EJ, Magid DJ; Adult Basic and Advanced Life Support, Pediatric Basic and Advanced Life Support, Neonatal Life Support, Resuscitation Education Science, and Systems of Care Writing Groups. Part 1: Executive Summary: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020 Oct 20;142(16_suppl_2):S337-S357. doi: 10.1161/CIR.0000000000000918. Epub 2020 Oct 21. PMID: 33081530.
- Stub D, Bernard S, Pellegrino V, Smith K, Walker T, Sheldrake J, Hockings L, Shaw J, Duffy SJ, Burrell A, Cameron P, Smit de V, Kaye DM. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO and early reperfusion (the CHEER trial). Resuscitation. 2015 Jan;86:88-94.
- Inoue A, Hifumi T, Sakamoto T, Kuroda Y. Extracorporeal Cardiopulmonary Resuscitation for Out-of-Hospital Cardiac Arrest in Adult Patients. J Am Heart Assoc. 2020 Apr 7;9(7):e015291. doi: 10.1161/JAHA.119.015291. Epub 2020 Mar 24. PMID: 32204668; PMCID: PMC7428656.


