Far-field R-wave (FFRW) reduction
Far-field R-wave (FFRW) reduction
Most of you will be familiar with FFR or fractional flow reserve, the term used frequently in interventional cardiology. But not so many would be familiar with Far-field R-wave reduction (FFRW), a terminology used in cardiac electrophysiology. Far-field R-wave sensing of the atrial lead of AAI or DDD pacemakers causes incorrect mode switches and is an important problem in patients with atrial arrhythmias in whom low voltage sensing is essential. AAI stands for atrial paced, atrial sensed and inhibited mode in pacemaker. DDD stands for dual chamber pacing, dual chamber sensing and dual response.
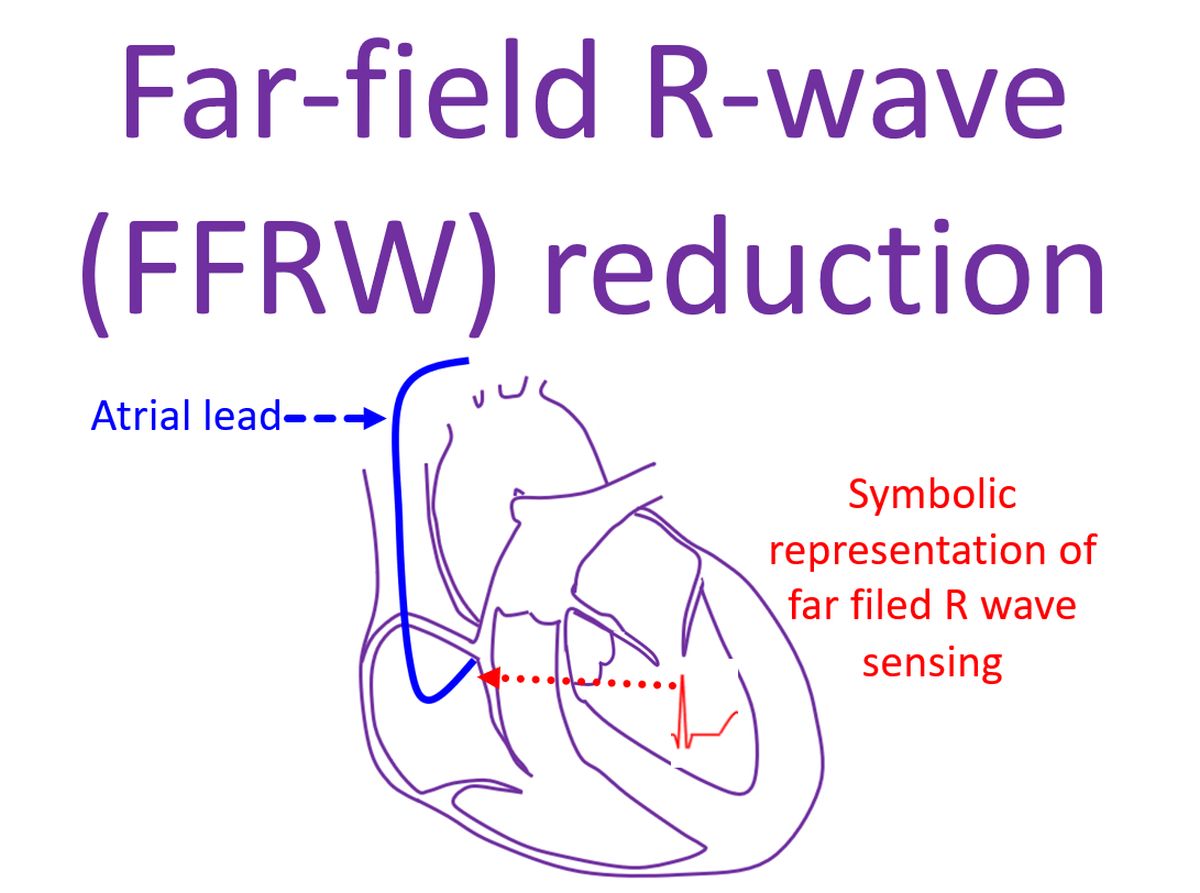
Far field sensing means sensing the ventricular electrogram by the atrial lead, which it is not supposed to do. If the atrial lead senses the R wave, it can be interpreted by the device as an atrial signal and get inhibited. In case of mode switching algorithms, far field sensing increases the number of ‘atrial signals’ counted and cause mode switches when actually there is no atrial fast rate which needs a mode switch to VVI. VVI is ventricular paced, ventricular sensed, inhibited mode. Mode switch in pacemakers is a protective mechanism to avoid high ventricular rates in cases like paroxysmal atrial fibrillation when there is also an indication for atrial based pacing.
De Groot JR et al tried to reduced FFRW by reducing the distance between the tip electrode and the proximal ring electrode of the atrial lead. They compared a short tip-ring distance of 1.1 mm with a conventional electrode with a larger tip-ring distance of 10 mm [1]. 36 patients with indication for DDD pacing were implanted with short tip-ring distance electrode while 23 patients were given conventional electrode. FFRW and P wave amplitudes sensed were measured during pacing and intrinsic rhythm at the time of implant. Repeat measurements were obtained at discharge and at follow up between 10 to 14 days after implantation.
P wave amplitude was slightly smaller in the short tip-ring distance electrode group, but was not statistically significant. There was a significant reduction in FFRW in the short tip-ring distance group during both intrinsic rhythm and pacing. The ratio between P wave and FFRW was much higher in the short tip-ring distance group (mean 48.6 vs 7.3). FFRW and P wave amplitudes did not change at hospital discharge or during follow up. This small study showed that FFRW can be suppressed without compromising P wave sensing using a short tip-ring distance, but needs further confirmation in studies checking clinical endpoints.
Similar results were reported in an earlier study of 15 patients and nine canines. The lead had center-to-center distance between the anode and cathode electrodes of 3.23 mm, which corresponded to an inter-electrode spacing of 1.1 mm. Follow up period in canines was 6 months. Positive results from the canine study prompted acute testing in humans scheduled for dual chamber pacing. P wave amplitudes were slightly smaller for the short tip-ring distance electrode, but not statistically significant. Mean FFRW voltage was significantly higher in conventional group compared to the short tip-ring distance group (mean 0.62 vs 0.10 mV). Pacing thresholds and impedances were comparable [2].
Another report had studied 10 mm tip-ring electrode distance at a time when 20 mm inter-electrode distance was also in use. They studied both FFRW and myopotential sensing in 66 patients. They noted FFRW sensing in 12 patients at an atrial sensitivity of 0.25 mV and an atrial blanking period of 50 ms. No FFRW was noted at an atrial sensitivity of 1.0 mV. Myopotentials were sensed in 3 patients. Measured P wave amplitude was at least twice the estimated amplitude of FFRW at an atrial blanking of 50 ms [3].
Locating the atrial lead at the Bachmann’s bundle region instead of right atrial appendage has also been shown to reduce FFRW. The study was in patients treated with multi-site atrial pacing. Right atrial lead implanted at the Bachmann’s bundle area in 69 patients was compared to right atrial appendage lead in 70 patients. Bachmann’s bundle is an interatrial bundle taking signals to the left atrium. At both atrial locations, bipolar sensing was superior to unipolar sensing in FFRW rejection, as expected. FFRW sensing occurred in 1% of patients at Bachmann’s bundle site compared to 11% at right atrial appendage site for bipolar sensing with sensitivity of 0.5 mV. This translated to a sensing safety margin of 5 or more in 99% of the Bachmann’s bundle group compared to 66% in the right atrial appendage group. This benefit was noted even in bipolar leads with 10 mm tip-ring electrode spacing [4].
FFRW sensing has also been investigated in Myotonic Dystrophy type 1 patients undergoing dual chamber pacemaker implantation, comparing positions at Bachmann’s bundle and right atrial appendage. There were 16 patients in the Bachmann’s bundle group and 18 in the conventional right atrial appendage group. Bipolar FFRW was lower than unipolar FFRW at both sites as expected. There were no significant differences between the sites in sensed P wave amplitude, atrial pacing and sensing thresholds and atrial lead impendence. Bachmann’s bundle region had the advantage of reducing oversensing of R wave on the atrial lead [5].
Incidentally, Bachmann’s bundle pacing has been shown to reduce atrial electromechanical delay in patients with type 1 myotonic dystrophy. Bachmann’s bundle pacing was done in the inter-atrial septum in the region of the Bachmann’s bundle. Both interatrial electromechanical delay and intra left atrial electromechanical delay were reduced during temporary Bachmann’s bundle pacing in the study of 70 patients. The study had a control group of 70 patients without type 1 Myotonic Dystrophy. Atrial electromechanical delay is an echocardiographic parameter correlated with the onset of supraventricular arrhythmias in several clinical conditions. Trans-thoracic echocardiogram with tissue Doppler (TDI) analysis was used in the study [6].
References
- De Groot JR, Schroeder-Tanka JM, Visser J, Willems AR, De Voogt WG. Clinical results of far-field R-wave reduction with a short tip-ring electrode. Pacing Clin Electrophysiol. 2008 Dec;31(12):1554-9. doi: 10.1111/j.1540-8159.2008.01226.x. PMID: 19067807.
- de Voogt W, van Hemel N, Willems A, Visser J, Chitre Y, Bornzin G, Helland J. Far-field R-wave reduction with a novel lead design: experimental and human results. Pacing Clin Electrophysiol. 2005 Aug;28(8):782-8. doi: 10.1111/j.1540-8159.2005.00175.x. PMID: 16105005.
- Nash A, Fröhlig G, Taborsky M, Stammwitz E, Maru F, Bouwens LH, Celiker C. Rejection of atrial sensing artifacts by a pacing lead with short tip-to-ring spacing. Europace. 2005 Jan;7(1):67-72. doi: 10.1016/j.eupc.2004.11.002. PMID: 15670970.
- Lewicka-Nowak E, Kutarski A, Dabrowska-Kugacka A, Rucinski P, Zagozdzon P, Raczak G. Atrial lead location at the Bachmann’s bundle region results in a low incidence of far field R-wave sensing. Europace. 2008 Feb;10(2):138-46. doi: 10.1093/europace/eum277. Epub 2008 Jan 11. PMID: 18192341.
- Russo V, Nigro G, Antonio Papa A, Rago A, Di Meo F, Cristiano A, Molino A, Calabrò R, Giovanna Russo M, Politano L. Far field R-wave sensing in Myotonic Dystrophy type 1: right atrial appendage versus Bachmann’s bundle region lead placement. Acta Myol. 2014 Oct;33(2):94-9. PMID: 25709379; PMCID: PMC4299168.
- Russo V, Rago A, Papa AA, Arena G, Politano L, Nigro G. Bachmann bundle pacing reduces atrial electromechanical delay in type 1 myotonic dystrophy patients. J Interv Card Electrophysiol. 2018 Apr;51(3):229-236. doi: 10.1007/s10840-018-0331-5. Epub 2018 Feb 27. PMID: 29488106.

