Heart failure in chronic kidney disease
Heart failure in chronic kidney disease
ക്രോണിക് കിഡ്നി ഡിസീസിൽ ഹാർട്ട് ഫെയ്ലർ
Prevalence of both heart failure and chronic kidney disease (CKD) are increasing [1]. Hence heart failure in chronic kidney disease is seen more often. Presence of CKD in heart failure increases morbidity and mortality. Though there is increasing use of evidence based drug and device therapy in heart failure patients in general, those with CKD have not been benefitted well [2].
The universal definition and classification of heart failure published in 2021 classifies heart failure as follows [3]. Heart failure with reduced ejection fraction (HFrEF) is defined as heart failure with a left ventricular ejection fraction of 40% or less. Heart failure with mildly reduced ejection fraction (HFmrEF) is heart failure with left ventricular ejection fraction from 41% to 49%. Heart failure with preserved ejection fraction (HFpEF) is heart failure with left ventricular ejection fraction of 50% or more.
CKD is defined as abnormalities of kidney structure or function, present for >3 months, with implications for health [4]. A more detailed definition is persistently reduced estimated glomerular filtration rate (eGFR) of <60 ml/min per 1.73 m2 or at least 1 marker of kidney damage for >3 months. The markers of kidney damage include albuminuria, urine sediment abnormalities, histological, or structural abnormalities detected on imaging. History of kidney transplantation is also included among markers of kidney damage. Significant albuminuria is albumin excretion rate of 30 mg/24 hours or more and albumin creatinine ratio of 30 mg/g or more [4, 5].
A few subgroups for heart failure in CKD have been described. They are HFpEF in nondialysis CKD, HFrEF in nondialysis CKD, HFpEF in dialysis-dependent CKD, HFrEF in dialysis-dependent CKD, and heart failure in kidney transplant patients [4].
Evidence for treatment with the major groups of medications used in mild-moderate CKD with heart failure have emerged from general population studies in patients with HFrEF [2]. Beta blockers have been shown to improve outcomes in patients with HFrEF in all stages of CKD. But those with severe CKD were excluded in studies on angiotensin converting enzyme inhibitors, angiotensin receptor blockers and mineralocorticoid receptor antagonists, as expected. Yet they have been useful in those with mild-moderate CKD and heart failure. Of course, close monitoring of renal status and a special watch for hyperkalemia is needed.
Angiotensin receptor neprilysin inhibitor therapy has been used successfully in randomized trials in patients with eGFR as low as 20 ml/min per 1.73 m2 . Treatment with sodium-glucose cotransporter inhibitor (SGLT2) improved mortality and hospitalization in patients with HFrEF and CKD stages 3 and 4, having eGFR>20 ml/min per 1.73 m2. Caution has to be exercised while using high dose combination diuretic therapy, often unavoidable in heart failure with CKD. They have the risk of worsening renal function and electrolyte imbalances. Intravenous iron therapy is another important aspect of treatment in patients with heart failure and CKD. High dose iron has been shown to reduce heart failure hospitalization by 44% in patients on dialysis. Improved symptoms have been noted in heart failure in stage 3 CKD [2].
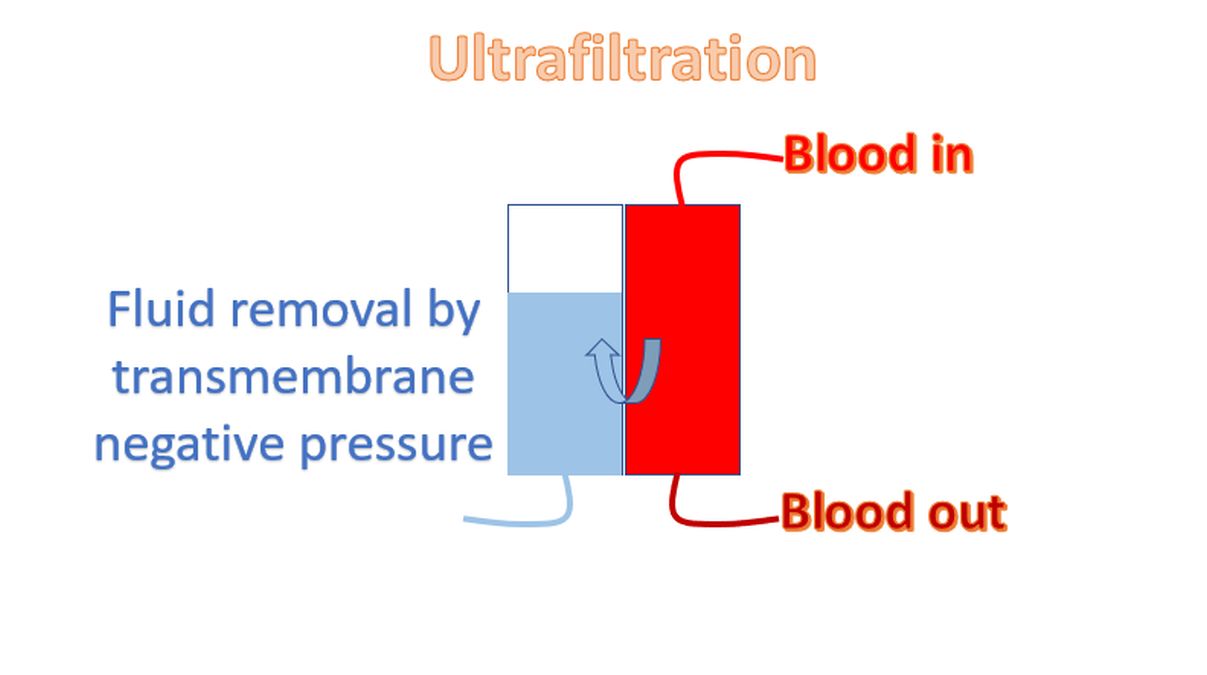
Another important aspect is cardiac resynchronization therapy in eligible patients with HFrEF and CKD. It has been shown to reduce mortality and hospitalizations in patients with heart failure and stage 3 CKD. Peritoneal dialysis can be used in patients with symptomatic fluid overload to improve symptoms and hospitalizations. Ultrafiltration is another useful option to remove excess fluid in heart failure patients on hemodialysis. Caution is needed to avoid hypotension due to excessive removal of fluid. A multidisciplinary approach combining cardiology and nephrology services is needed for optimal management of heart failure in patients with CKD. Of course it is a usual decision in multi-system ailments in medical practice.
References
- House AA, Wanner C, Sarnak MJ, Piña IL, McIntyre CW, Komenda P, Kasiske BL, Deswal A, deFilippi CR, Cleland JGF, Anker SD, Herzog CA, Cheung M, Wheeler DC, Winkelmayer WC, McCullough PA; Conference Participants. Heart failure in chronic kidney disease: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2019 Jun;95(6):1304-1317. doi: 10.1016/j.kint.2019.02.022. Epub 2019 Apr 30. PMID: 31053387.
- Banerjee D, Rosano G, Herzog CA. Management of Heart Failure Patient with CKD. Clin J Am Soc Nephrol. 2021 Jul;16(7):1131-1139. doi: 10.2215/CJN.14180920. Epub 2021 Jan 25. PMID: 33495289; PMCID: PMC8425606.
- Bozkurt B, Coats AJ, Tsutsui H, Abdelhamid M, Adamopoulos S, Albert N, Anker SD, Atherton J, Böhm M, Butler J, Drazner MH, Felker GM, Filippatos G, Fonarow GC, Fiuzat M, Gomez-Mesa JE, Heidenreich P, Imamura T, Januzzi J, Jankowska EA, Khazanie P, Kinugawa K, Lam CSP, Matsue Y, Metra M, Ohtani T, Francesco Piepoli M, Ponikowski P, Rosano GMC, Sakata Y, SeferoviĆ P, Starling RC, Teerlink JR, Vardeny O, Yamamoto K, Yancy C, Zhang J, Zieroth S. Universal Definition and Classification of Heart Failure: A Report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure. J Card Fail. 2021 Mar 1:S1071-9164(21)00050-6. doi: 10.1016/j.cardfail.2021.01.022. Epub ahead of print. PMID: 33663906.
- Chapter 1: Definition and classification of CKD. Kidney Int Suppl (2011). 2013 Jan;3(1):19-62. doi: 10.1038/kisup.2012.64. PMID: 25018975; PMCID: PMC4089693.
- House AA, Wanner C, Sarnak MJ, Piña IL, McIntyre CW, Komenda P, Kasiske BL, Deswal A, deFilippi CR, Cleland JGF, Anker SD, Herzog CA, Cheung M, Wheeler DC, Winkelmayer WC, McCullough PA; Conference Participants. Heart failure in chronic kidney disease: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2019 Jun;95(6):1304-1317. doi: 10.1016/j.kint.2019.02.022. Epub 2019 Apr 30. PMID: 31053387.



