Penetrating aortic ulcer (PAU)
Penetrating aortic ulcer (PAU)
Penetrating aortic ulcer (PAU) is one of the three important acute aortic syndromes, the other two being acute aortic dissection and intramural hematoma. Majority of the PAU occur in the descending thoracic aorta, which contributes to about sixty percent while nearly one third occur in the abdominal aorta [1]. Only around six percent are seen in the aortic arch. About half of the ulcers are isolated, without any associated intramural hematoma or saccular aneurysms. Nearly one fourth have associated saccular aneurysms while about a seventh of them have associated intramural hematoma.
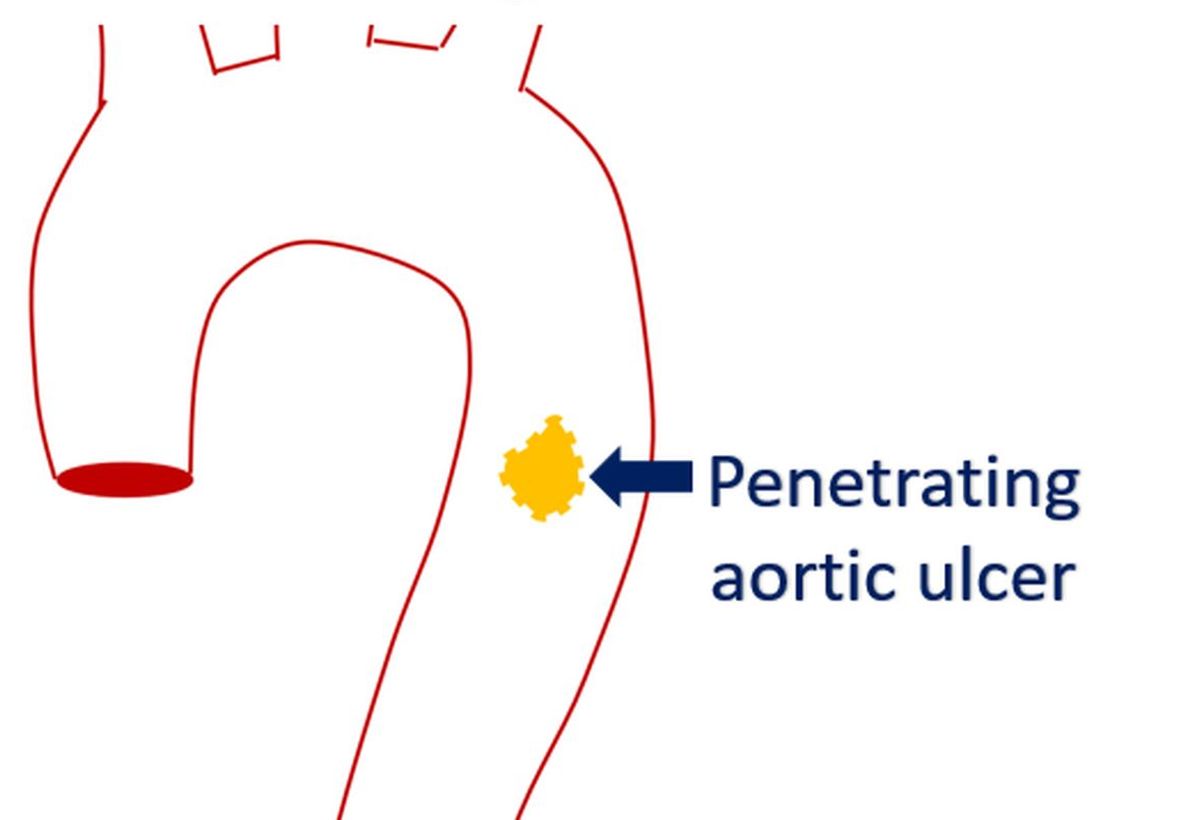
Penetrating aortic ulcer is an ulceration of an atheromatous plaque that extends deeply beyond the aortic intima and into the aortic media. Important complications of PAU include aortic intramural hematoma, aortic dissection, pseudoaneurysm formation or even aortic rupture. Pseudoaneurysm is usually due to rupture of the ulcer into the adventitia [2]. Symptomatic ulcers are more likely to progress than an incidentally detected asymptomatic penetrating aortic ulcer.
Penetrating aortic ulcer usually occurs in the elderly with hypertension and may present with chest pain or pain in the back. Unlike in aortic dissection, pulse deficit, stroke, aortic regurgitation or compromise of a branch vessel are not seen. Recurrence of symptoms while on conservative medical treatment may mandate other forms of treatment like surgical intervention [2].
Computed tomographic (CT) angiography is the investigation of choice for the diagnosis of PAU. The ulcer is seen as an projection of contrast material from the aortic lumen. Volume rendered three dimensional reconstruction of CT aortogram gives an excellent demonstration of the ulcers and any associated hematoma or aortic dissection.
Progression is more likely in a symptomatic aortic ulcer. Ulcers with 20 mm or more maximum diameter or maximum depth 10 mm or more have a high risk of progression. They should be considered for early surgical or endovascular repair [3]. Symptomatic aortic ulcers are better treated with endovascular aortic repair (EVAR) than surgery, mostly due to their age and associated comorbidities.
References
-
- Nathan DP et al. Presentation, complications, and natural history of penetrating atherosclerotic ulcer disease. J Vasc Surg. 2012 Jan;55(1):10-5.
- Cooke JP, Kazmier FJ, Orszulak TA. The penetrating aortic ulcer: pathologic manifestations, diagnosis, and management. Mayo Clin Proc. 1988 Jul;63(7):718-25. doi: 10.1016/s0025-6196(12)65534-7. PMID: 3386311.
- Ganaha F et al. Prognosis of aortic intramural hematoma with and without penetrating atherosclerotic ulcer: a clinical and radiological analysis. Circulation 2002;106:342-348.



