Important aspects of pulmonary embolism
Important aspects of pulmonary embolism
Pulmonary embolism is a potentially life threatening condition which needs prompt recognition and treatment. Venous thromboembolism presenting as deep vein thrombosis or pulmonary embolism is the third most frequent acute cardiovascular syndrome, the other two being myocardial infarction and stroke. A few cases of paradoxical pulmonary embolism secondary to aortocaval fistula associated with an abdominal aortic aneurysm with thrombus has been reported. Aortocaval fistula can occur in an abdominal aortic aneurysm secondary to spontaneous rupture, following trauma or surgery. Aortocaval fistula created during interventional procedures are closed immediately after the procedure with a device. Since pulmonary embolism is a very vast topic, only some aspects are being covered in this discussion.
The commonest ECG finding in acute pulmonary embolism is sinus tachycardia. T wave inversion in anterior leads is another finding in pulmonary embolism. Incomplete right bundle branch block pattern can also be a manifestation sometimes noted in pulmonary embolism. Both the anterior T wave inversion and incomplete right bundle branch block pattern are indicative of the acute right ventricular overload due to obstruction of pulmonary circulation. ECG changes of acute right ventricular overload resolve rapidly with the resolution of pulmonary embolism by treatment and may return to near normal levels as the pulmonary arterial pressure normalizes.
S1Q3T3 pattern is the classical ECG pattern of acute pulmonary embolism which is often taught in ECG classes, though it is not the commonest ECG finding in pulmonary embolism [1]. S1Q3T3 pattern means the presence of an S wave in lead I, indicating a rightward shift of QRS axis, with Q wave and T inversion in lead III. The same pattern can also occur in other cases of acute cor pulmonale.
There are some named radiological signs in pulmonary embolism. Westermark sign is a focal oligemia of the lung due to occlusion of a branch pulmonary artery due to pulmonary embolism. The vessel proximal to the occlusion is dilated. Hampton’s hump is a peripheral pleural based wedge shaped lung opacity due to pulmonary infarction in a case of pulmonary embolism. Knuckle sign is the abrupt cut off of a pulmonary artery branch due to pulmonary embolism.
Echocardiography is an important tool in the initial bedside evaluation of suspected acute pulmonary embolism. Visualization of thrombi within the right heart or pulmonary arteries would be the most direct way of diagnosing acute pulmonary embolism by echocardiography. Mobile thrombi in the right heart (Taenia cordis) detected during echocardiography also carries a poor prognosis with higher association with right ventricular dysfunction and mortality. In general, the chance of detection of mobile right heart thrombi in acute pulmonary embolism is about 4%, though up to 18% have been detected in certain intensive care settings. Trans esophageal echo can detect thrombi in central pulmonary arteries as well. Hence it may be a useful investigation when patient is too unstable to be shifted for computerized tomographic pulmonary angiography [2,3]. Echocardiography is also useful in differential diagnosis by demonstrating an alternate diagnosis like massive pericardial effusion with cardiac tamponade or aortic dissection.
Emergency bedside echocardiogram is useful in documenting right ventricular enlargement and increase in right ventricular systolic pressure. Right ventricular systolic pressure will be equal to pulmonary artery pressure in the absence of pulmonary stenosis. McConnell sign and 60/60 sign may be present on echocardiography. McConnell’s sign is akinesia of right ventricular mid-free wall with sparing of apex seen in acute pulmonary embolism. This finding has a sensitivity of 77% and specificity of 94% [4]. A potential false positive situation is right ventricular myocardial infarction [5].
60/60 sign in acute pulmonary embolism is a pattern detected by Doppler echocardiography indicating a disturbed right ventricular ejection pattern.
The sign has two components:
- Tricuspid regurgitation jet gradient of less than 60 mm Hg, corresponding to TR velocity less than 3.9 m/s
- Pulmonary flow acceleration time of less than 60 ms [6,7].
It may be noted that TR gradient should be above 30 mm Hg to indicate pulmonary hypertension due to pulmonary embolism. High TR gradients may indicate chronic thromboembolic pulmonary hypertension, especially in presence of right ventricular free wall hypertrophy suggesting long standing pulmonary hypertension. False positive results have been noted in pulmonary fibrosis and acute respiratory distress following lung resection [4]. 60/60 sign has been noted to have a sensitivity of 25% and specificity of 94% in one study [5]
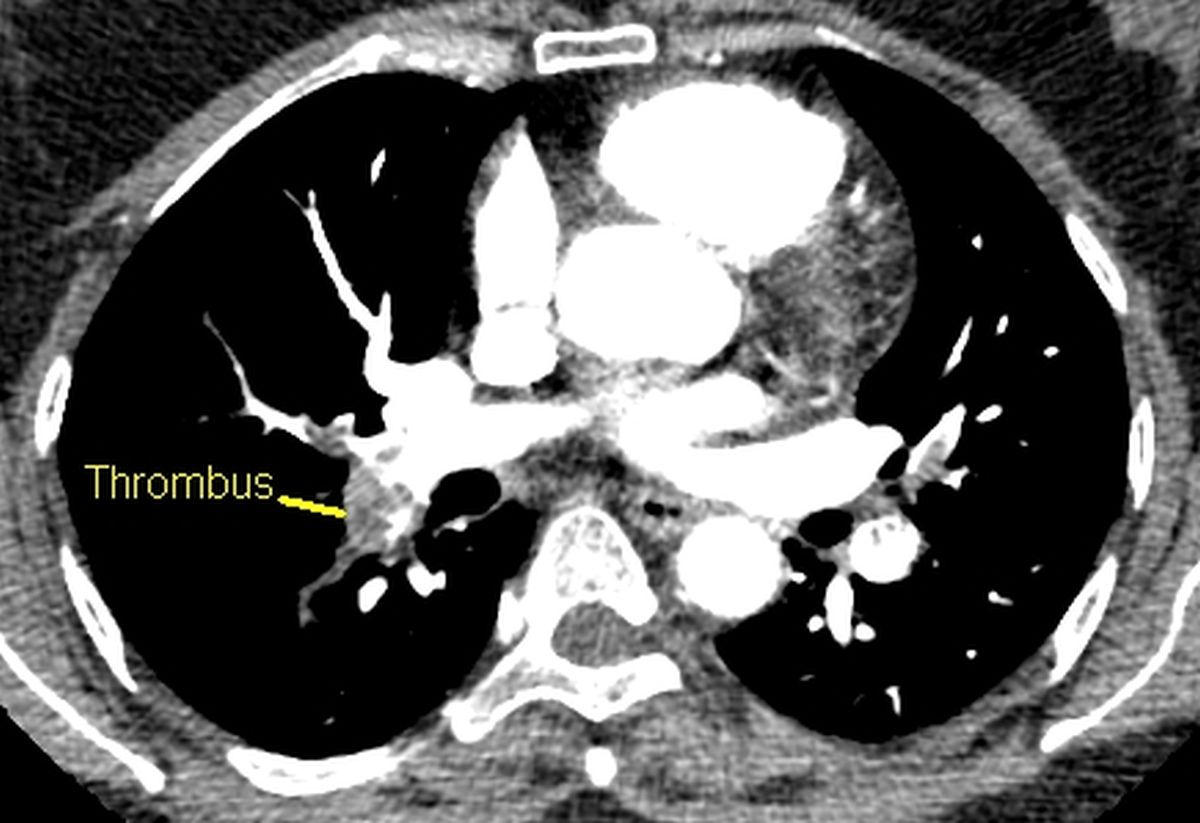
Eminent demonstration of pulmonary thrombus has made computed tomographic (CT) pulmonary angiography the gold standard in the diagnosis of pulmonary thromboembolism. If CT pulmonary angiogram is negative one can safely conclude that currently there is no pulmonary embolism, though rarely a recent embolus may have got fragmented and resolved.
Contrast enhanced CT scan of thorax below shows a filling defect in the right branch pulmonary artery. The density is like that of a thrombus.
Medications approved for the treatment of normotensive pulmonary embolism are heparin, fondaparinux, rivaroxaban, apixaban, dabigatran and edoxaban. Dabigatran is a direct thrombin inhibitor while rivaroxaban, apixaban and edoxaban are oral factor Xa inhibitors. Fondaparinux is a parenteral factor Xa inhibitor. Role of non-vitamin K antagonists for secondary prevention is gradually taking over the time old vitamin K antagonists. Thrombolytic therapy is reserved for rescue in case of decompensation due to right ventricular failure or recurrence of pulmonary embolism in these stable patients.
Classic role for thrombolytic therapy is for massive pulmonary embolism with hypotension. Now the role is being expanded to those with right ventricular dysfunction and elevated troponin. Thrombolytic therapy leads to faster improvement in pulmonary obstruction and pulmonary arterial pressures compared to unfractionated heparin alone. Though the greatest benefit is obtained when treatment is started within 48 hours of onset of symptoms, it can still be useful in those with symptoms for 6 to 14 days [8].
Rheolytic thrombectomy has been reported when there is contraindication to systemic thrombolysis in patients with pulmonary embolism and right ventricular dysfunction [9]. It is combined with local thrombolysis delivered through the catheter directly into the occluded pulmonary artery. The device used for rheolytic thrombectomy is the Angiojet catheter which is a dual lumen 100 cm catheter which fragments and aspirates thrombi using the Bernoulli principle. It is introduced through a long sheath which is introduced through the femoral vein into the pulmonary artery. One lumen of the Angiojet catheter carries high velocity high pressure saline jet that is aspirated back through the other lumen. The resulting low pressure vortex macerates and aspirates the thrombus back through the return lumen.
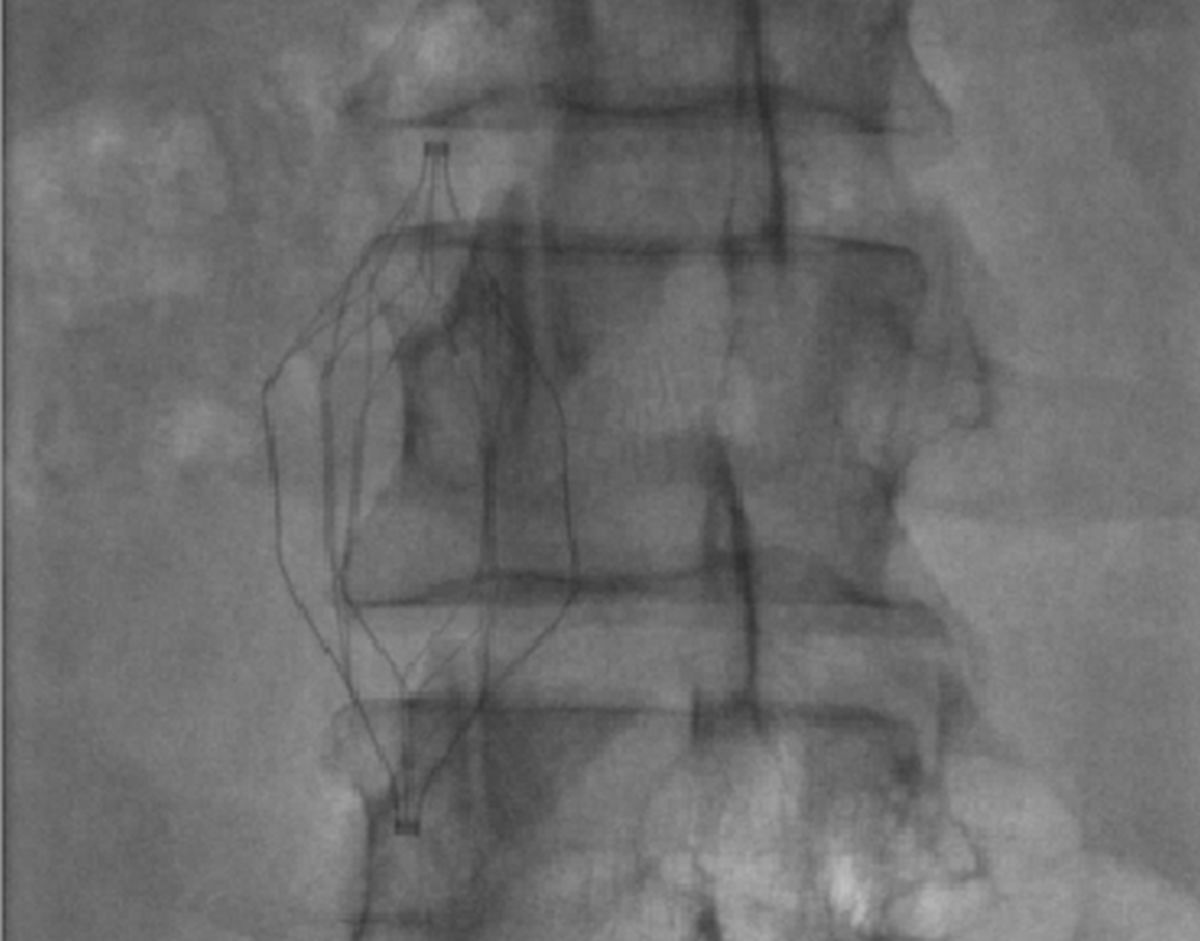
Inferior vena caval filters are deployed for prevention of pulmonary embolism in the face of venous thrombosis. It is considered for secondary prophylaxis after an episode of massive pulmonary embolism. The filter deployment can be either temporary (retrievable filter) or permanent. Inferior vena caval filter (IVC filter) deployment is favoured when there are contraindications for anticoagulant therapy. IVC filter can also be temporarily deployed for prevention of pulmonary embolism while thrombolysing deep vein thrombosis, especially when a large mobile clot has been demonstrated by ultrasound evaluation.
References
- Petruzzelli S, Palla A, Pieraccini F, Donnamaria V, Giuntini C. Routine electrocardiography in screening for pulmonary embolism. Respiration. 1986;50(4):233-43.
- Torbicki A, Galie` N, Covezzoli A, Rossi E, De Rosa M, Goldhaber SZ. Right heart thrombi in pulmonary embolism: results from the International Cooperative Pulmonary Embolism Registry. J Am Coll Cardiol 2003;41(12):2245 – 2251.
- Casazza F, Bongarzoni A, Centonze F, Morpurgo M. Prevalence and prognostic significance of right-sided cardiac mobile thrombi in acute massive pulmonary embolism. Am J Cardiol 1997;79(10):1433 – 1435.
- McConnell MV, Solomon SD, Rayan ME, Come PC, Goldhaber SZ, Lee RT. Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism. Am J Cardiol. 1996 Aug 15;78(4):469-73. doi: 10.1016/s0002-9149(96)00339-6. PMID: 8752195.
- Casazza F, Bongarzoni A, Capozi A, Agostoni O. Regional right ventricular dysfunction in acute pulmonary embolism and right ventricular infarction. Eur J Echocardiogr. 2005 Jan;6(1):11-4.
- Lodato JA, Ward RP, Lang RM. Echocardiographic predictors of pulmonary embolism in patients referred for helical CT. Echocardiography. 2008 Jul;25(6):584-90.
- Kurzyna M, Torbicki A, Pruszczyk P, Burakowska B, Fijałkowska A, Kober J, Oniszh K, Kuca P, Tomkowski W, Burakowski J, Wawrzyńska L. Disturbed right ventricular ejection pattern as a new Doppler echocardiographic sign of acute pulmonary embolism. Am J Cardiol. 2002 Sep 1;90(5):507-11.
- Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, Huisman MV, Humbert M, Jennings CS, Jiménez D, Kucher N, Lang IM, Lankeit M, Lorusso R, Mazzolai L, Meneveau N, Áinle FN, Prandoni P, Pruszczyk P, Righini M, Torbicki A, Van Belle E, Zamorano JL; The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur Respir J. 2019 Oct 9;54(3):1901647. doi: 10.1183/13993003.01647-2019. PMID: 31473594.
- Ferrigno L, Bloch R, Threlkeld J, Demlow T, Kansal R, Karmy-Jones R. Management of pulmonary embolism with rheolytic thrombectomy. Can Respir J. 2011 Jul-Aug;18(4):e52-8. doi: 10.1155/2011/614953. PMID: 22059183; PMCID: PMC3205106.

