Intra aortic balloon pump (IABP)
Intra aortic balloon pump (IABP)
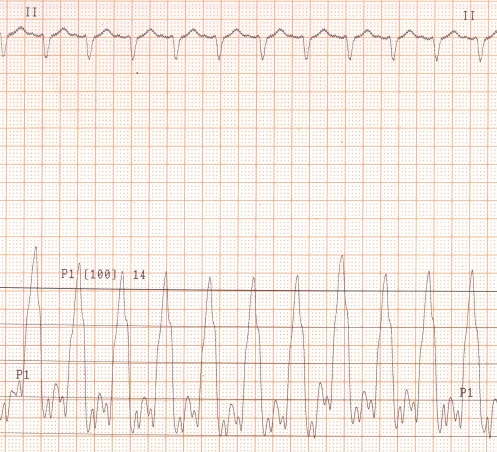
Pressure tracing and ECG while on intra aortic balloon counterpulsation. The upper channels shows the ECG and the lower channel shows the arterial pressure tracing. It can be clearly seen that the diastolic pressure (after the T wave on the electrocardiogram) is much higher than the systolic pressure. This is because the intra aortic balloon is inflated in diastole and deflated in systole. IABP is inserted to support the left ventricle and to reduce the after load. Inflation of the balloon in diastole enhances the coronary perfusion and is very useful in cardiogenic shock due to myocardial infarction. The balloon is inserted percutaneously through the femoral artery. The upper part of the balloon is kept below the left subclavian artery in the descending thoracic aorta. The lower part is above the renal arteries. The balloon size is chosen according to the size of the individual to meet the above criteria.
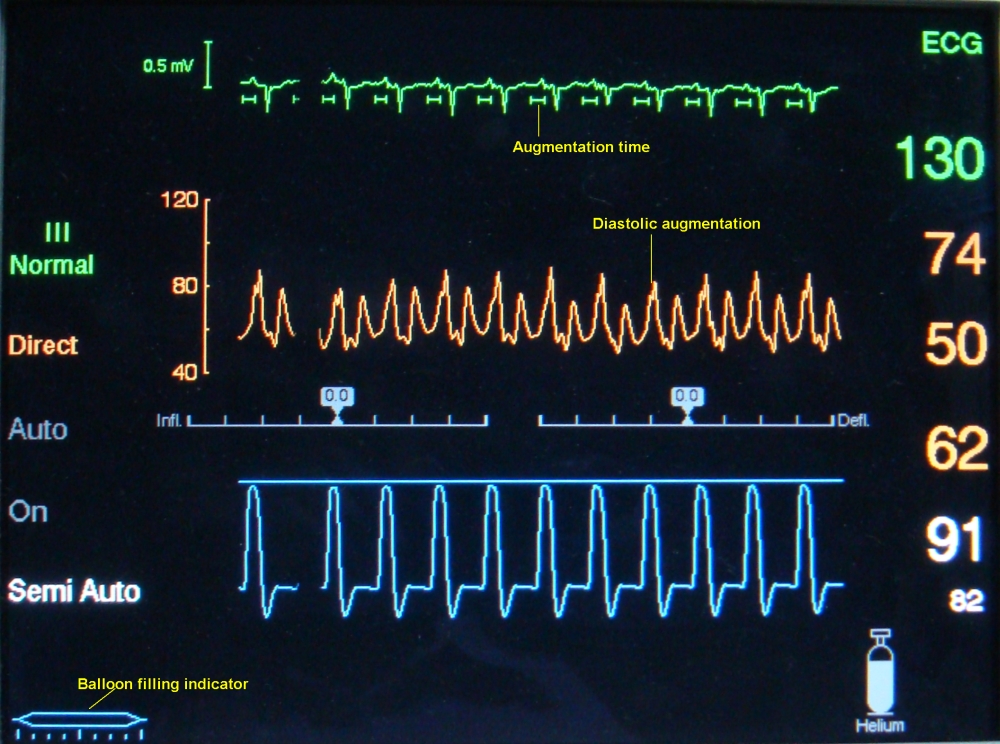
The uppermost green tracing is the electrocardiogram which is used to time the inflation and deflation of the balloon. The augmentation time is marked just below the tracing to indicate the exact point of inflation and deflation. The arterial pressure tracing just below that indicates the diastolic augmentation. The figure on the top in green colour (130) indicates the heart rate. The figures below are the peak, trough and mean pressures from the arterial line. Augmentation level and alarm limit for the augmentation are the lower figures. The filling level of the helium tank is also indicated. The diagram of the graduated balloon will show the filling in real time by the flickering of light on and off. Helium is used for filling the balloon because it is the lightest inert gas which can move in and out rapidly according to the cardiac cycle. Balloon inflation and deflation can be triggered either by the ECG or by the pressure tracing. In auto mode the choice is done by the circuitry automatically. Here the augmentation ratio is 1:1, meaning that all cycles receive augmentation. It can be reduced while weaning off like augmentation of alternate cycles or lower.
IABP will not work in the presence of significant aortic regurgitation. Significant aortic disease is another contraindication for the insertion of an IABP.
In IABP-SHOCK II trial, IABP did not reduce 30 day mortality compared to control. This resulted in international guideline recommendation for IABP use in cardiogenic shock complicating acute myocardial infarction to be downgraded. The trial randomized 600 patients with cardiogenic shock complication acute myocardial infarction who were undergoing early revascularization to either IABP or control [1]. At 12 month follow up, 52% in the IABP group and 51% in the control group had died. There were no significant differences in reinfarction, recurrent revascularization or stroke. Quality of life measures among the survivors also did not differ significantly between the groups. 6 year follow up data also did not show any mortality benefit for those who were randomly assigned to receive IABP support [2]. But mortality was very high, with two thirds of patients with cardiogenic shock dying even with revascularization and optimal medical therapy.
References
-
Thiele H, Zeymer U, Neumann FJ, Ferenc M, Olbrich HG, Hausleiter J, de Waha A, Richardt G, Hennersdorf M, Empen K, Fuernau G, Desch S, Eitel I, Hambrecht R, Lauer B, Böhm M, Ebelt H, Schneider S, Werdan K, Schuler G; Intraaortic Balloon Pump in cardiogenic shock II (IABP-SHOCK II) trial investigators. Intra-aortic balloon counterpulsation in acute myocardial infarction complicated by cardiogenic shock (IABP-SHOCK II): final 12 month results of a randomised, open-label trial. Lancet. 2013 Nov 16;382(9905):1638-45.
- Thiele H, Zeymer U, Thelemann N, Neuman F, Hausleiter J, Abdel-Wahab M, Meyer-Saraei R, Fuernau G, Eitel C, Hambrecht R, Bohm M, Werdan K, Felix SB, Hennersdorf M, Schneider S, Ouarrak T, Desch S, de Waha-Thiele S. Intra-aortic balloon pump in cardiogenic shock complicating acute myocardial infarction: long-term 6-year outcome of the randomized Intraaortic Balloon Pump in cardiogenic shock II (IABP-SHOCK II) Trial.Circulation. 2018;138:395–403.