Is CT or invasive coronary angiography preferable in stable chest pain?
Is CT or invasive coronary angiography preferable in stable chest pain?
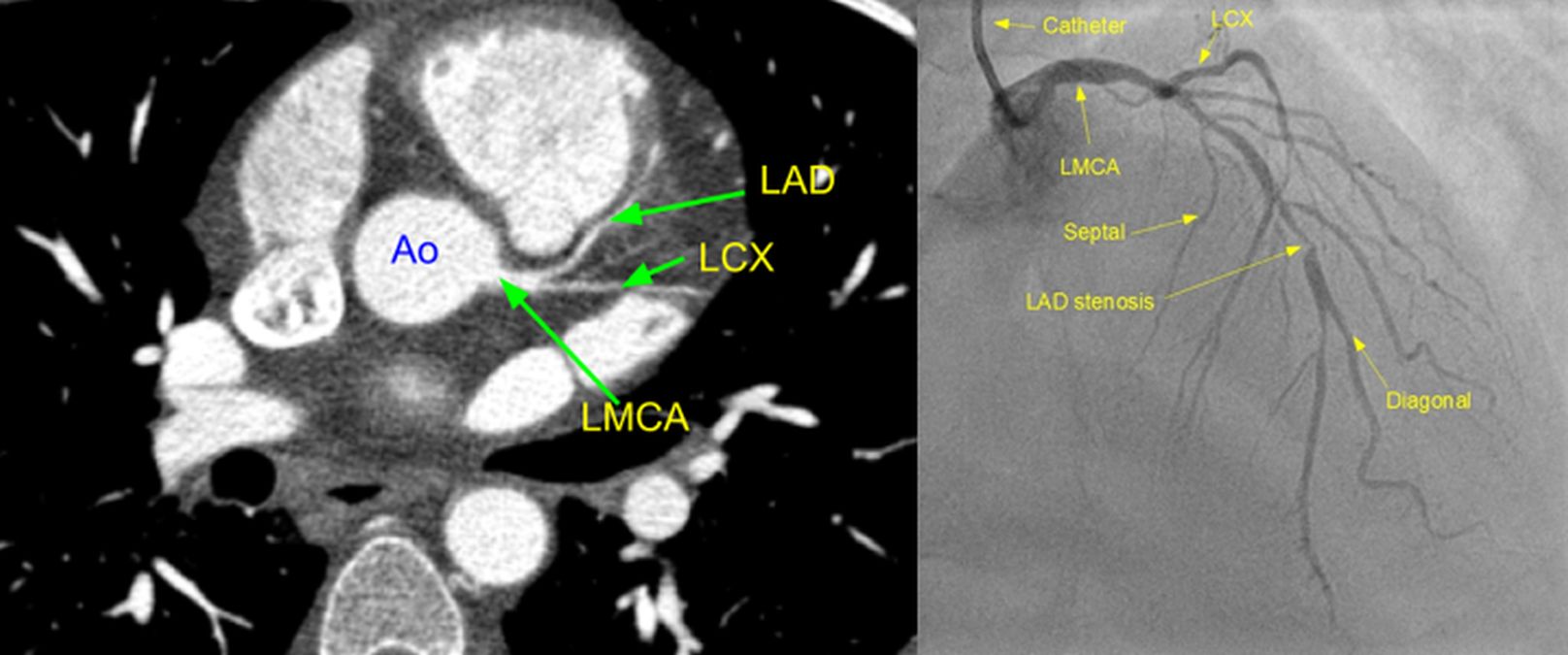
Patients with chest pain suggestive of angina pectoris generally undergo invasive coronary angiography and revascularization if feasible. Threshold for coronary angiography may vary from region to region, depending on availability of resources. Non-invasive testing in the form of treadmill exercise ECG or sometimes a nuclear imaging stress test/stress echocardiography may be done prior to coronary angiography to look for evidence of inducible ischemia. But these tests are neither hundred percent sensitive or nor specific. Computed tomographic (CT) coronary angiogram is another modality which is considered prior to invasive coronary angiography in the recent era. The DISCHARGE Trial Group compared the two as the initial strategy in a study published in The New England Journal of Medicine, on March 4, 2022 [1].
It was a randomized trial comparing CT coronary angiography and invasive coronary angiography as initial diagnostic strategies for guiding treatment of persons with stable chest pain and an intermediate pretest probability of obstructive coronary artery disease. The study was done across 26 European centres. Primary outcome assessed was major adverse cardiovascular events of cardiovascular death, nonfatal myocardial infarction or nonfatal stroke over 3.5 years of follow up. Main secondary outcomes noted were procedure related complications and angina pectoris.
Complete follow up could be obtained from 3523 of the 3561 study patients. Major procedure related complications occurred in 0.5% of the CT coronary angiography group and 1.9% of the invasive coronary angiography group. Angina during the final 4 weeks of follow-up was reported in 8.8% of the CT group and 7.5% in the invasive coronary angiography group. Major adverse cardiovascular events occurred in 2.1% of the CT group and 3% of the invasive group. Authors concluded that in the intermediate pretest probability group, the risk of major adverse cardiovascular events was similar in both groups. Major procedure related complications were lower in the initial CT strategy.
An accompanying editorial pointed out certain issues with the trial [2]. There were only limited number of patients with high-risk anatomy who would benefit from revascularization, 13.9% in CT group and 11.2% in the initial invasive coronary angiography group. Pretest probability cut off for the trial was 10-60% in this trial. More than 35% had non-anginal chest pain (37.4% in the CT group and 36.2% in the invasive group). These two trial design features could have led to the observation that only a quarter of the patients had obstructive coronary artery disease with luminal narrowing of 50% or more. This might suggest that the trial group was actually low risk rather than intermediate risk. The editorial author also pointed out that ACC/AHA guidelines published in 2021 does not recommend testing in the low risk group [3]. CT based fractional flow reserve (FFRCT) [4] and quantification of plaque burden and lesion characteristics might improve the accuracy of prediction [5]. It may be noted that many lesions leading to acute coronary events are not flow limiting before plaque activation.
References
- Maurovich-Horvat P, Bosserdt M, Kofoed KF, Rieckmann N, Benedek T, Donnelly P, Rodriguez-Palomares J, Erglis A, Štěchovský C, Šakalyte G, Čemerlić Adić N, Gutberlet M, Dodd JD, Diez I, Davis G, Zimmermann E, Kępka C, Vidakovic R, Francone M, Ilnicka-Suckiel M, Plank F, Knuuti J, Faria R, Schröder S, Berry C, Saba L, Ruzsics B, Kubiak C, Gutierrez-Ibarluzea I, Schultz Hansen K, Müller-Nordhorn J, Merkely B, Knudsen AD, Benedek I, Orr C, Xavier Valente F, Zvaigzne L, Suchánek V, Zajančkauskiene L, Adić F, Woinke M, Hensey M, Lecumberri I, Thwaite E, Laule M, Kruk M, Neskovic AN, Mancone M, Kuśmierz D, Feuchtner G, Pietilä M, Gama Ribeiro V, Drosch T, Delles C, Matta G, Fisher M, Szilveszter B, Larsen L, Ratiu M, Kelly S, Garcia Del Blanco B, Rubio A, Drobni ZD, Jurlander B, Rodean I, Regan S, Cuéllar Calabria H, Boussoussou M, Engstrøm T, Hodas R, Napp AE, Haase R, Feger S, Serna-Higuita LM, Neumann K, Dreger H, Rief M, Wieske V, Estrella M, Martus P, Dewey M. CT or Invasive Coronary Angiography in Stable Chest Pain. N Engl J Med. 2022 Mar 4. doi: 10.1056/NEJMoa2200963. Epub ahead of print. PMID: 35240010.
- Loscalzo J. Evaluating Stable Chest Pain – An Evolving Approach. N Engl J Med. 2022 Mar 4. doi: 10.1056/NEJMe2201446. Epub ahead of print. PMID: 35240011.
- Gulati M, Levy PD, Mukherjee D, Amsterdam E, Bhatt DL, Birtcher KK, Blankstein R, Boyd J, Bullock-Palmer RP, Conejo T, Diercks DB, Gentile F, Greenwood JP, Hess EP, Hollenberg SM, Jaber WA, Jneid H, Joglar JA, Morrow DA, O’Connor RE, Ross MA, Shaw LJ. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Nov 30;144(22):e368-e454. doi: 10.1161/CIR.0000000000001029. Epub 2021 Oct 28. Erratum in: Circulation. 2021 Nov 30;144(22):e455. PMID: 34709879.
- Douglas PS, De Bruyne B, Pontone G, Patel MR, Norgaard BL, Byrne RA, Curzen N, Purcell I, Gutberlet M, Rioufol G, Hink U, Schuchlenz HW, Feuchtner G, Gilard M, Andreini D, Jensen JM, Hadamitzky M, Chiswell K, Cyr D, Wilk A, Wang F, Rogers C, Hlatky MA; PLATFORM Investigators. 1-Year Outcomes of FFRCT-Guided Care in Patients With Suspected Coronary Disease: The PLATFORM Study. J Am Coll Cardiol. 2016 Aug 2;68(5):435-445. doi: 10.1016/j.jacc.2016.05.057. PMID: 27470449.
- Andreini D, Conte E, Serruys PW. Coronary plaque features on CTA can identify patients at increased risk of cardiovascular events. Curr Opin Cardiol. 2021 Nov 1;36(6):784-792. doi: 10.1097/HCO.0000000000000917. PMID: 34620793.
