Polyphasic or splintered QRS in Ebstein’s anomaly
Polyphasic or splintered QRS in Ebstein’s anomaly of tricuspid valve
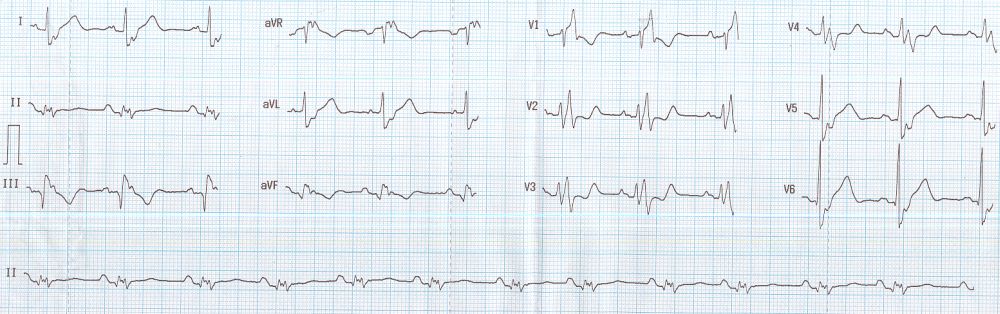
ECG in Ebstein’s anomaly of tricuspid valve showing right bundle branch block (RBBB) pattern with polyphasic and splintered QRS. The QRS is wide and Lead V2 shows rsrs pattern mimicking right bundle branch block. Lead II shows multiple small deflections (splintered QRS). The slurred S waves in lateral leads also form part of the RBBB pattern.
The duration of QRS has been linked to right ventricular enlargement and dysfunction in Ebstein’s anomaly. A larger atrialized right ventricular volume has been noted in these cases. As a corollary, those with near normal ECG would have mild morphological abnormalities and a better clinical profile [1].
Splintered and polyphasic QRS of Ebstein’s anomaly can also be considered as fragmented QRS as per the new terminology. Fragmented QRS is a marker of myocardial scar and consequent arrhythmias in ischemic and nonischemic cardiomyopathy. Similarly fragmented QRS has been shown to be associated with larger region of atrialized right ventricle and increased risk of arrhythmic events in Ebstein’s anomaly [2].
Ebstein’s anomaly may be associated with right sided accessory pathway in ventricular pre-excitation (WPW syndrome) with or without atrioventricular re-entrant tachycardia. Multiple accessory pathways can occur and radiofrequency catheter ablation is effective [3].
Rare cases of ventricular tachycardia with Ebstein’s anomaly have also been reported in literature. One was a case of sustained monomorphic ventricular tachycardia and received an implantable cardioverter defibrillator [4]. Peritricuspid reentry has been documented in another case of ventricular tachycardia in Ebstein’s anomaly [5]. Scar formation in the inferior atrialized portion of the right ventricle formed the substrate for the re-entrant ventricular tachycardia in this case. Yet another young girl with Ebstein’s anomaly and ventricular tachycardia received an entirely subcutaneous defibrillator [6].
Tall P waves due to gross right atrial enlargement in Ebstein’s anomaly have been called Himalayan P waves, though not seen in the ECG illustrated here [7]. Himalayan P waves are also described in tricuspid atresia [8].
References
- Egidy Assenza G, Valente AM, Geva T, Graham D, Pluchinotta FR, Sanders SP, Autore C, Volpe M, Landzberg MJ, Cecchin F. QRS duration and QRS fractionation on surface electrocardiogram are markers of right ventricular dysfunction and atrialization in patients with Ebstein anomaly. Eur Heart J. 2013 Jan;34(3):191-200.
- Park SJ, Chung S, On YK, Kim JS, Yang JH, Jun TG, Jang SY, Lee OJ, Song J, Kang IS, Huh J. Fragmented QRS complex in adult patients with Ebstein anomaly and its association with arrhythmic risk and the severity of the anomaly. Circ Arrhythm Electrophysiol. 2013 Dec;6(6):1148-55.
- Wei W, Zhan X, Xue Y, Fang X, Liao H, Deng H, Liang Y, Wu S. Features of accessory pathways in adult Ebstein’s anomaly. Europace. 2014 Nov;16(11):1619-25.
- Baztarrica GE, Sereno GG, Villecco SA, Porcile R. Ventricular tachycardia an atypical presentation of Ebstein’s disease. Saudi Med J. 2014 Dec;35(12):1510-2.
- Kumar S, Subramanian A, Selvaraj RJ. Peritricuspid reentrant ventricular tachycardia in Ebstein’s anomaly. Europace. 2014 Nov;16(11):1633.
- Cipolletta L, Luzi M, Piangerelli L, Guerra F, Capucci A. Entirely subcutaneous implantable defibrillator: safest option in a young girl with ventricular tachycardia and Ebstein anomaly. Circ Arrhythm Electrophysiol. 2014 Apr;7(2):358-9.
- Sharma V, Sharma A, Kumar V. Himalayan P waves. Intern Emerg Med. 2011 Feb;6(1):81-2.
- Reddy SC, Zuberbuhler JR. Images in cardiovascular medicine. Himalayan P-waves in a patient with tricuspid atresia. Circulation. 2003 Jan 28;107(3):498.

