Right Heart Catheterization in Tetralogy of Fallot
Right Heart Catheterization in Tetralogy of Fallot
With the availability of high resolution echocardiographic images and Doppler echocardiography, role of cardiac catheterization has come down in tetralogy of Fallot and other congenital heart diseases in general. Important risks for cardiac catheterization in a deeply cyanotic infant are the chance of precipitation of a cyanotic spell and thrombotic strokes due to hemoconcentration. Chance of precipitating a cyanotic spell are more when pulmonary angiography is attempted through the already narrow right ventricular outflow tract. Hemocontration is due to the diuresis following contrast angiography, which can be prevented by adequate pre and post procedure hydration.
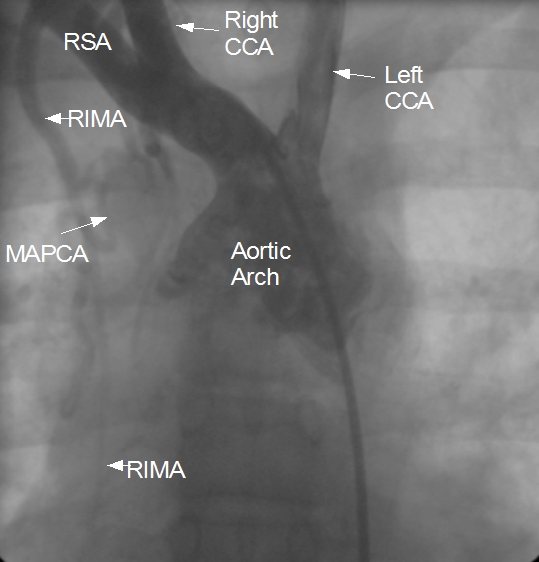
Diagnostic cardiac catheterization may be needed especially in tetralogy of Fallot with pulmonary atresia, to assess the pulmonary anatomy, including size and distribution of peripheral pulmonary arteries. Major aortopulmonary collateral arteries (MAPCAs) can be delineated by angiography during right heart catheterization. The image shows a MAPCA originating from right internal mammary artery. Finding out the origin and insertion of MAPCAs is important prior to surgical repair of tetralogy of Fallot. Another important role is for detection of coronary anomalies, which can also be seen on echocardiogram sometimes. Magnetic resonance imaging is another way of documenting coronary anomalies.
McGoon’s ratio is calculated by dividing the sum of diameters of right and left pulmonary arteries by diameter of aorta at the level of diaphragm. Normal subjects have a value around 2.1. In cases of tetralogy of Fallot, a ratio above 1.2 is associated with acceptable post repair right ventricular systolic pressure. If McGoon’s ratio is below 0.8, initial shunt surgery is an option to allow the pulmonary artery branches to grow in size and for a later complete repair of tetralogy of Fallot [1]. If the pulmonary anatomy is poor, there will be post repair right ventricular hypertension, which is deleterious and has long term seqeulae.
Findings which are sought during an aortogram in tetralogy of Fallot include looking for aortic regurgitation, coronary anomalies, MAPCAs, patent ductus arteriosus and side of the aortic arch. All of these are important while planning palliative and definitive surgical repair. Classic Blalock Taussig shunt (BT shunt) used to be done on the side opposite to that of the aortic arch so that the presence of brachiocephalic trunk prevents kinking of the subclavian artery which is mobilized down to anastomose with the pulmonary artery branch on the same side. Anomalous coronary arteries can cross the right ventricular outflow tract and can be damaged during procedures needed for widening of the RVOT.
Beyond diagnostic right heart catheterization, palliative transcatheter interventions are useful both pre and post operatively in tetralogy of Fallot. Stenting of the patent ductus arteriosus can be considered in neonatal period for improving oxygen saturation till corrective surgery. Procedures for enlarging the right ventricular outflow tract and perforation of an atretic membrane in pulmonary atresia have been described. Post operatively there could be branch pulmonary artery stenosis, residual right ventricular outflow tract obstruction, pulmonary regurgitation or residual left to right shunts noted during long term follow up. Transcatheter interventions can palliate these conditions and avoid or delay the need for reoperation [2].
References
- Wagdy R. The role of diagnostic cardiac catheterization for children with congenital heart diseases: local experience. Arch Med Sci Atheroscler Dis. 2018 Jun 28;3:e72-e79. doi: 10.5114/amsad.2018.76824. PMID: 30775593; PMCID: PMC6374569.
- Stapleton GE. The role of cardiac catheterisation in patients with tetralogy of Fallot. Cardiol Young. 2013 Dec;23(6):883-7. doi: 10.1017/S1047951113001777. PMID: 24401262.

