Right ventricular infarction
Right ventricular infarction
Right ventricular infarction can be associated with inferior wall infarction. It is due to occlusion of the right ventricular branches of the right coronary artery. The actual prevalence of right ventricular infarction may be underestimated because right sided chest leads are not part of routine 12 lead ECG. In a study which included right sided chest leads V3R, V4R, V5R and V6R, ST elevation of 1 mm or more in any of these leads was found to be a reliable sign of right ventricular involvement. It was a study of 67 patients who underwent serial electrocardiograms and 99mtechnetium pyrophosphate scintigraphy and a dynamic flow study to document right ventricular infarction [1]. They noted that ST elevation of 1 mm or more in V4R had the greatest sensitivity of 93% and predictive accuracy (93%) for right ventricular myocardial infarction. Of special interest was the observation that ST segment elevation in right precordial leads was short lived, disappearing in 10 hours in half of the patients with right ventricular infarction. So recording right chest leads within 10 hours of onset of chest pain is important in picking up right ventricular infarction.
Right ventricular infarction decreases its output and consequently the left ventricular preload leading to a decrease in cardiac output. Profound hypotension can be noted in some cases. The ischemic right ventricle is stiff and volume dependent [2], thereby explaining the role of fluid resuscitation in right ventricular infarction with hypotension. Cardiac output can be enhanced by right atrial contraction which increases right ventricular filling, if the coronary occlusion is distal to the origin of right atrial branches. But more proximal occlusion results in impaired right ventricular filling and performance due to the loss of right atrial help. Bradycardia which is often associated with inferior wall infarction also limit the cardiac output in this situation.
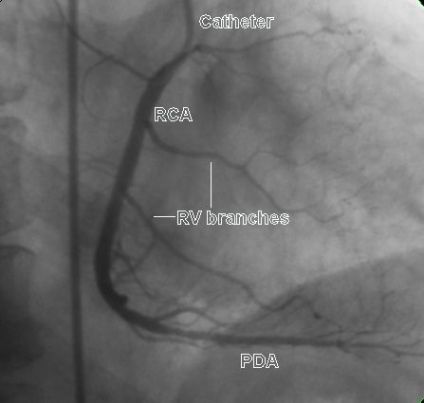
Here is a right coronary angiogram showing right ventricular branches:
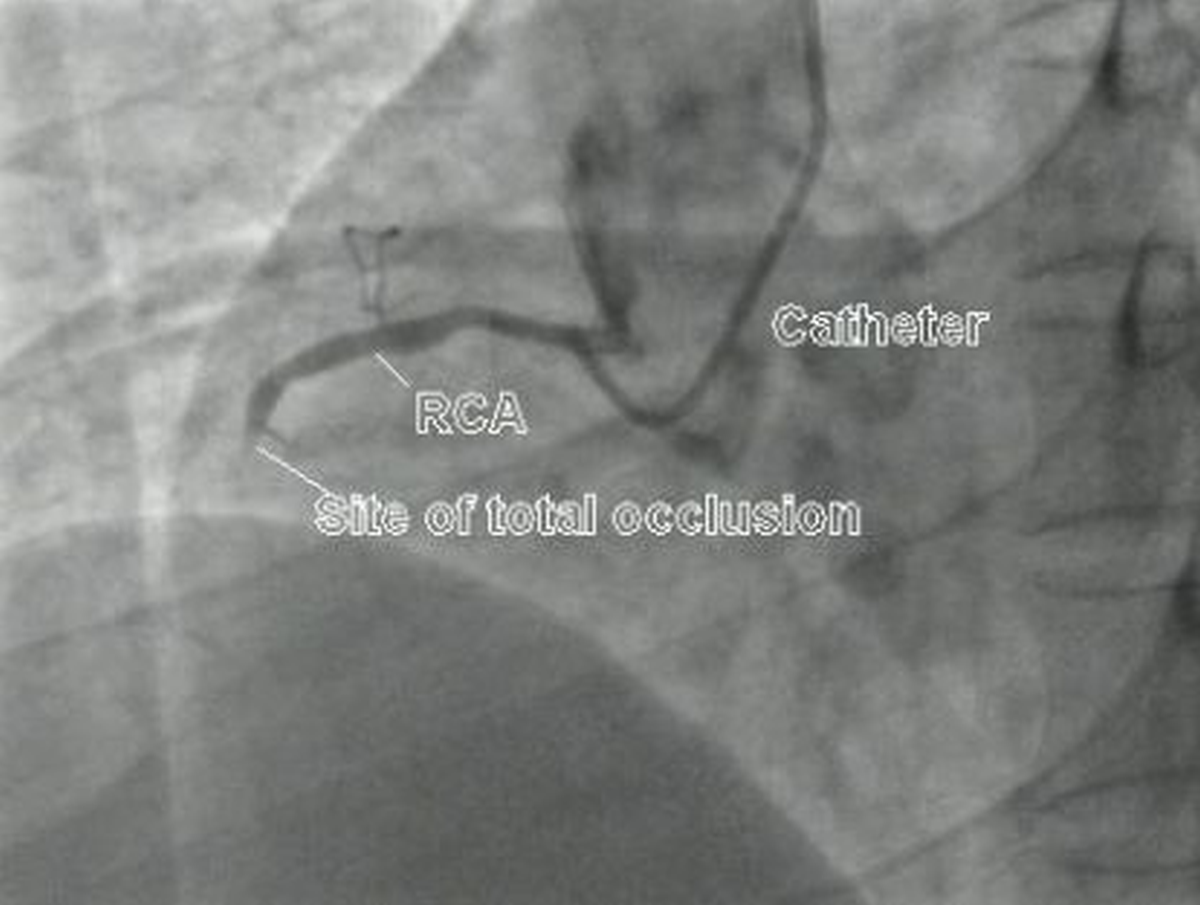
Relatively proximal total occlusion of right coronary artery is shown here. Hardly any right ventricular branches are seen. A small branch is seen just proximal to the occlusion, and another more proximally. These could be right atrial branches. Right atrium is usually supplied by an anterior artery which often gives rise to the sinus node artery and a lateral artery which supplies the right atrial free wall [3].
The term right ventricular “infarction” has been called as a misnomer because most of the right ventricular dysfunction is due to ischemic but viable myocardium [2]. Right ventricle is perfused both in systole and diastole unlike the left ventricle, because of the lower intracavitary systolic pressure. Thin right ventricular wall can also derive oxygenation from the blood in the cavity as well as through Thebesian veins, even in the presence of coronary occlusion. Generally right ventricular function recovers even in the absence of reperfusion. But the recovery can be slow and associated with high in hospital mortality. Of course, reperfusion enhances recovery and improves clinical course and survival.
Inferior wall infarction generally has a good prognosis with only 2-9% mortality in the control group of trials on thrombolytic therapy. But presence of associated right ventricular infarction makes it a high risk entity [4]. Clinically right ventricular infarction has hypotension, elevated jugular venous pressure which is usually 10 cm or more with a positive Kussmaul’s sign. Kussmaul’s sign is an inspiratory increase in jugular venous pressure, instead of the normal fall. Lung fields are clear as there is no elevation of pulmonary capillary pressure. Tricuspid regurgitation may be present. Clinical signs may be absent in many cases.
Early recognition of right ventricular infarction is important as the usually used nitrate therapy can lead to hypotension in the presence of right ventricular infarction. Instead volume loading, and dobutamine or dopamine if needed, may be considered.
Those with right ventricular infarction along with inferior wall infarction have a high risk of developing high grade atrioventricular block. High grade AV block was noted in 14 of 29 patients (48%) with right ventricular involvement documented by 99m-technetium pyrophosphate scintigraphy. In the same study, only 5 out of 38 patients (13%) with inferior wall infarction and no right ventricular involvement had high grade AV block [5]. Atrioventricular sequential pacing rather than ventricular temporary pacing has been advocated by some in inferior wall infarction with right ventricular infarction and complete heart block. The potential risk of perforation of the ischemic right ventricle in this scenario in a patient often restless due to hypotension and cerebral hypoperfusion has to be kept in mind.
Complete reperfusion of the right coronary artery by percutaneous coronary intervention can lead to excellent recovery of right ventricular function and excellent clinical outcome. Unsuccessful reperfusion is associated with impaired recovery of right ventricular function with hemodynamic compromise and high mortality rate [6].
References
- Braat SH, Brugada P, de Zwaan C, Coenegracht JM, Wellens HJ. Value of electrocardiogram in diagnosing right ventricular involvement in patients with an acute inferior wall myocardial infarction. Br Heart J. 1983 Apr;49(4):368-72.
- Goldstein JA. Pathophysiology and management of right heart ischemia. J Am Coll Cardiol. 2002 Sep 4;40(5):841-53.
- Busquet J, Fontan F, Anderson RH, Ho SY, Davies MJ. The surgical significance of the atrial branches of the coronary arteries. Int J Cardiol. 1984 Aug;6(2):223-36.
- Berger PB, Ryan TJ. Inferior myocardial infarction. High-risk subgroups. Circulation. 1990 Feb;81(2):401-11.
- Braat SH, de Zwaan C, Brugada P, Coenegracht JM, Wellens HJ. Right ventricular involvement with acute inferior wall myocardial infarction identifies high risk of developing atrioventricular nodal conduction disturbances. Am Heart J. 1984 Jun;107(6):1183-7.
- Bowers TR, O’Neill WW, Grines C, Pica MC, Safian RD, Goldstein JA. Effect of reperfusion on biventricular function and survival after right ventricular infarction. N Engl J Med. 1998 Apr 2;338(14):933-40.
