Rupture of sinus of Valsalva aneurysm (RSOV)
Rupture of sinus of Valsalva aneurysm (RSOV)
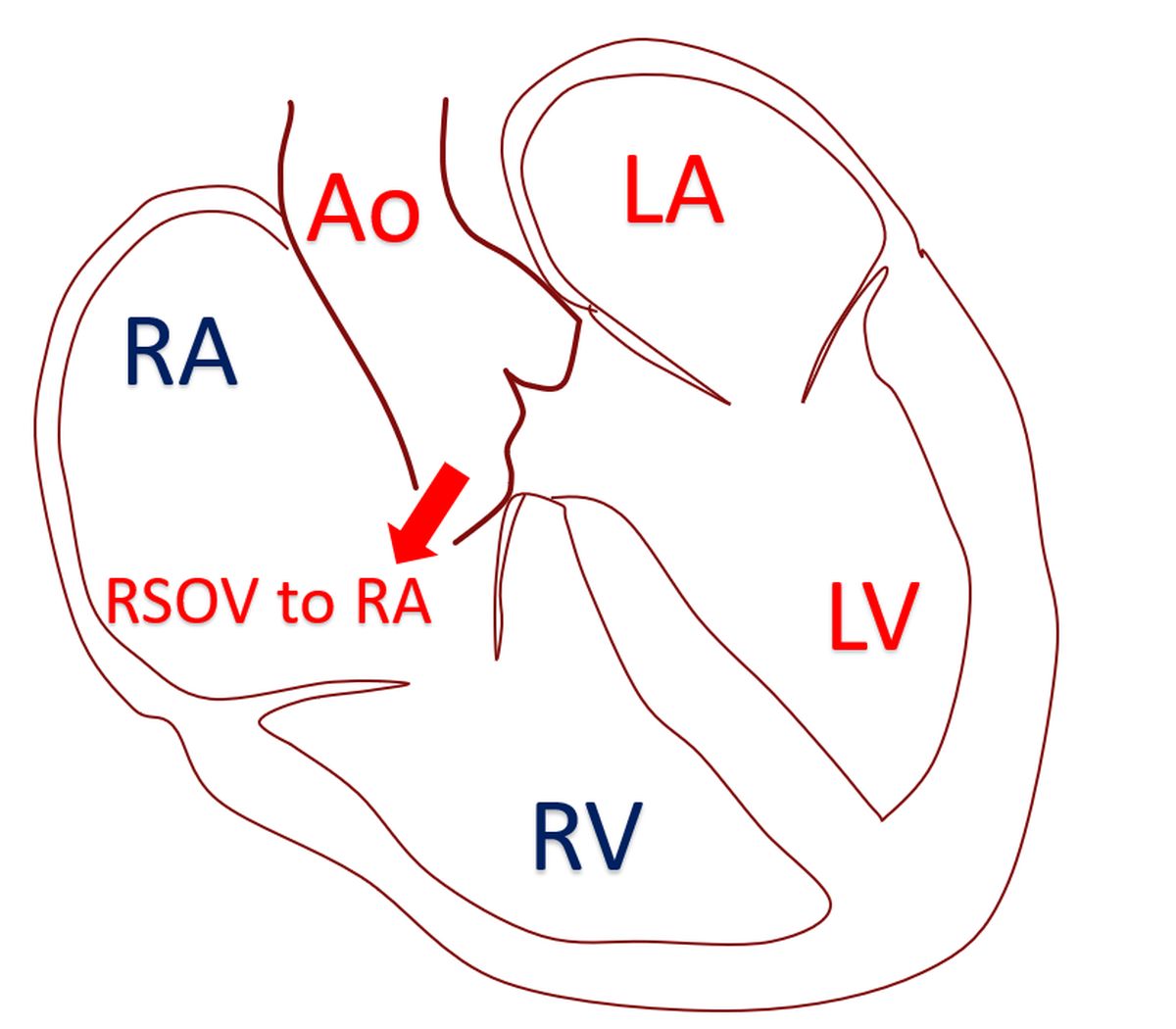
Sinus of Valsalva aneurysm is usually due to a defect in the aortic media. A ventricular septal defect or aortic regurgitation may be found as associated abnormalities. Nearly 70% of aneurysms originate from the right coronary sinus [1]. The aneurysm may compress an adjacent chamber, coronary artery or conduction system. These can cause myocardial ischemia or conduction disturbances. About one third of aneurysms rupture and produce acute symptoms in a quarter of patients [2]. Important symptoms following rupture are dyspnea, chest pain and fatigue. If it ruptures into the right sided chambers, it produces a left to right shunt. The severity of shunt and associated lesions determine the severity of symptoms [3].
Rupture of sinus of Valsalva aneurysm (RSOV) usually occurs into the right heart chambers. Rarely rupture can occur into left heart chambers, pericardium, pulmonary artery or superior vena cava [3]. Rupture into the pericardium can cause cardiac tamponade [4]. The classical clinical finding in RSOV to right ventricle is a continuous murmur with diastolic augmentation. The aneurysm track through the right ventricular wall gets compressed during systole and flow is better in diastole, causing the diastolic augmentation of murmur. Rupture into the left ventricle will cause only a diastolic murmur.
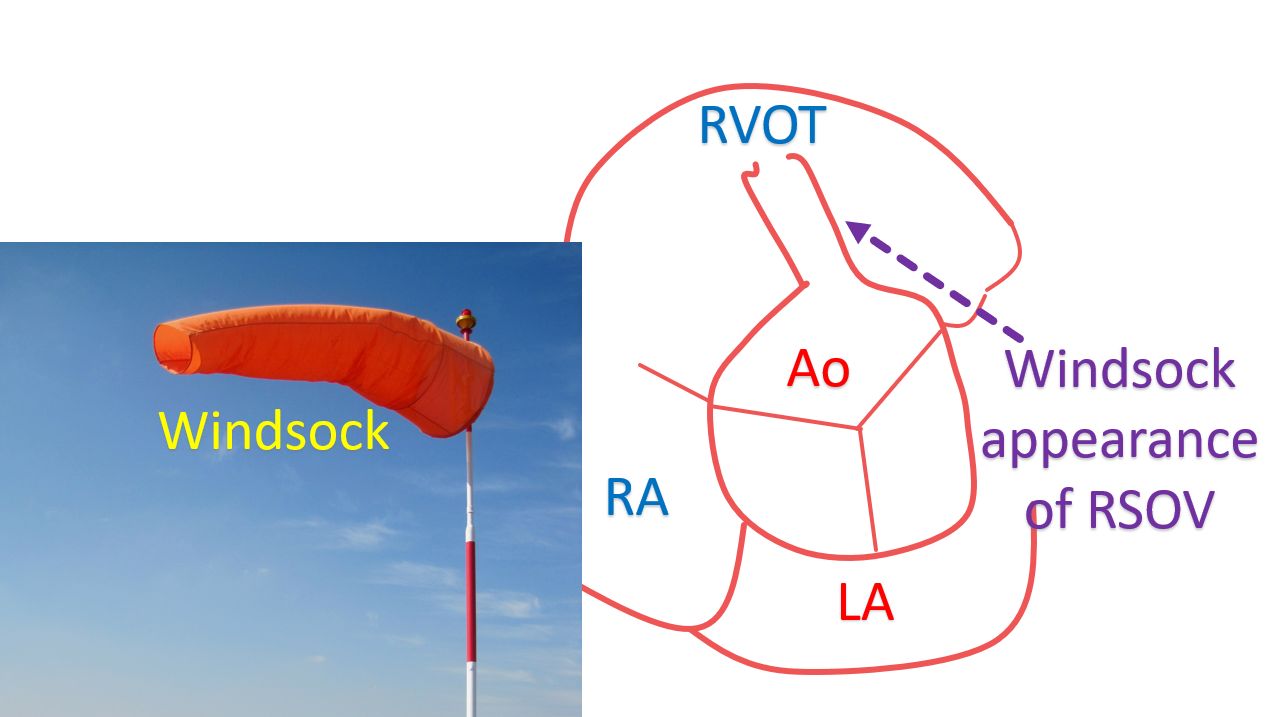
Echocardiography and magnetic resonance imaging are two important investigations for RSOV. Transesophageal echocardiography may give more details than a transthoracic echocardiogram. Occasionally a sinus of Valsalva aneurysm may be detected prior to rupture as well. The classical echocardiographic appearance in RSOV to RV is a ‘windsock appearance’, of the aneurysm in the right ventricular outflow tract. Windsock appearance is better seen on transesophageal echocardiography [5].
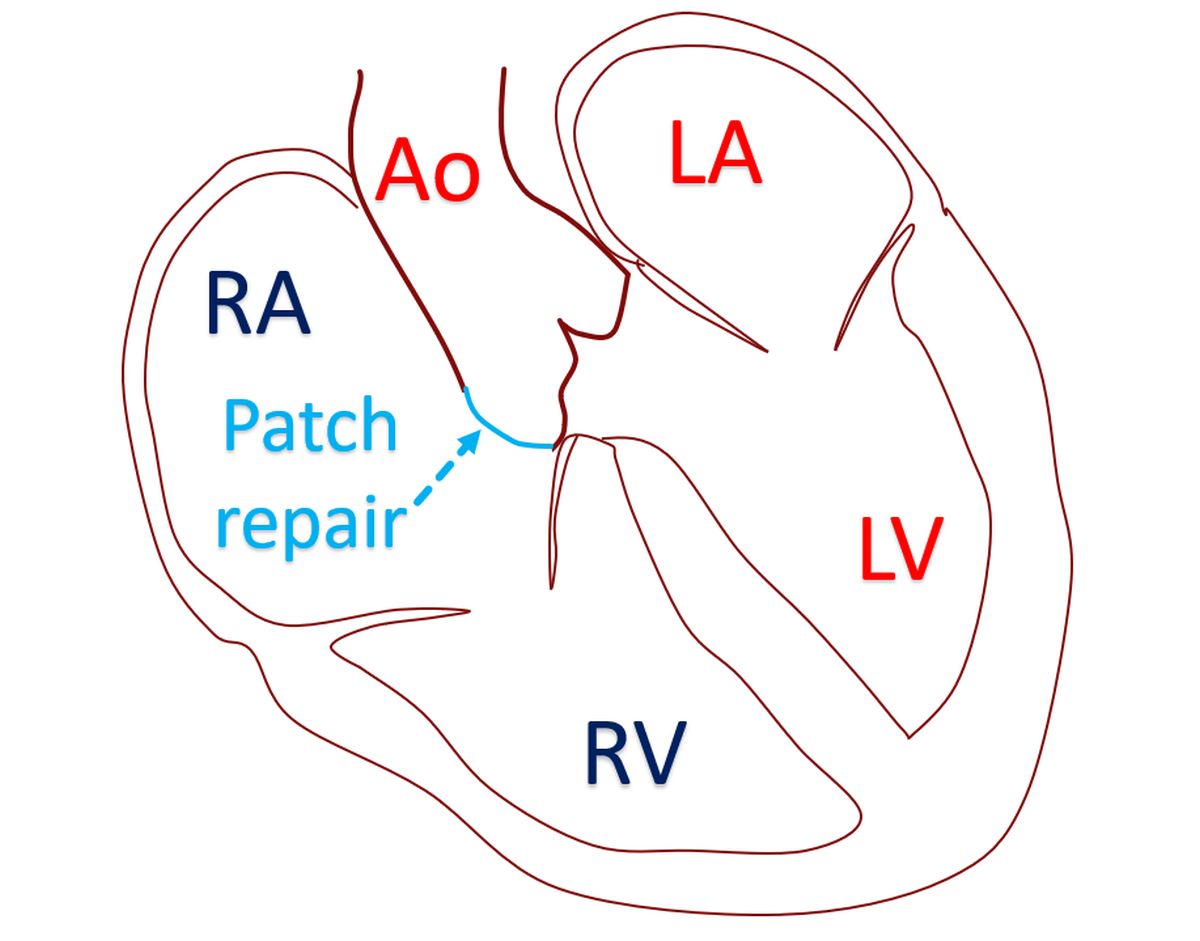
Cardiac catheterization is seldom needed for diagnosis and coronary angiography may be done pre-operatively prior to surgical repair. The first successful surgical closure of RSOV was reported by Lillehei et al in 1957 [6]. Surgery is usually by dual exposure technique with both aorta and the chamber of termination being explored. The aneurysmal sac is removed and the defect repaired either by direct suture or patch closure. Associated lesions like ventricular septal defect and aortic regurgitation will be tackled in the same surgical sitting. Aortic valve replacement may be needed in some cases [2]. A purely transaortic repair of RSOV may cause postoperative aortic regurgitation by progressive distortion of the aortic sinus geometry [7].
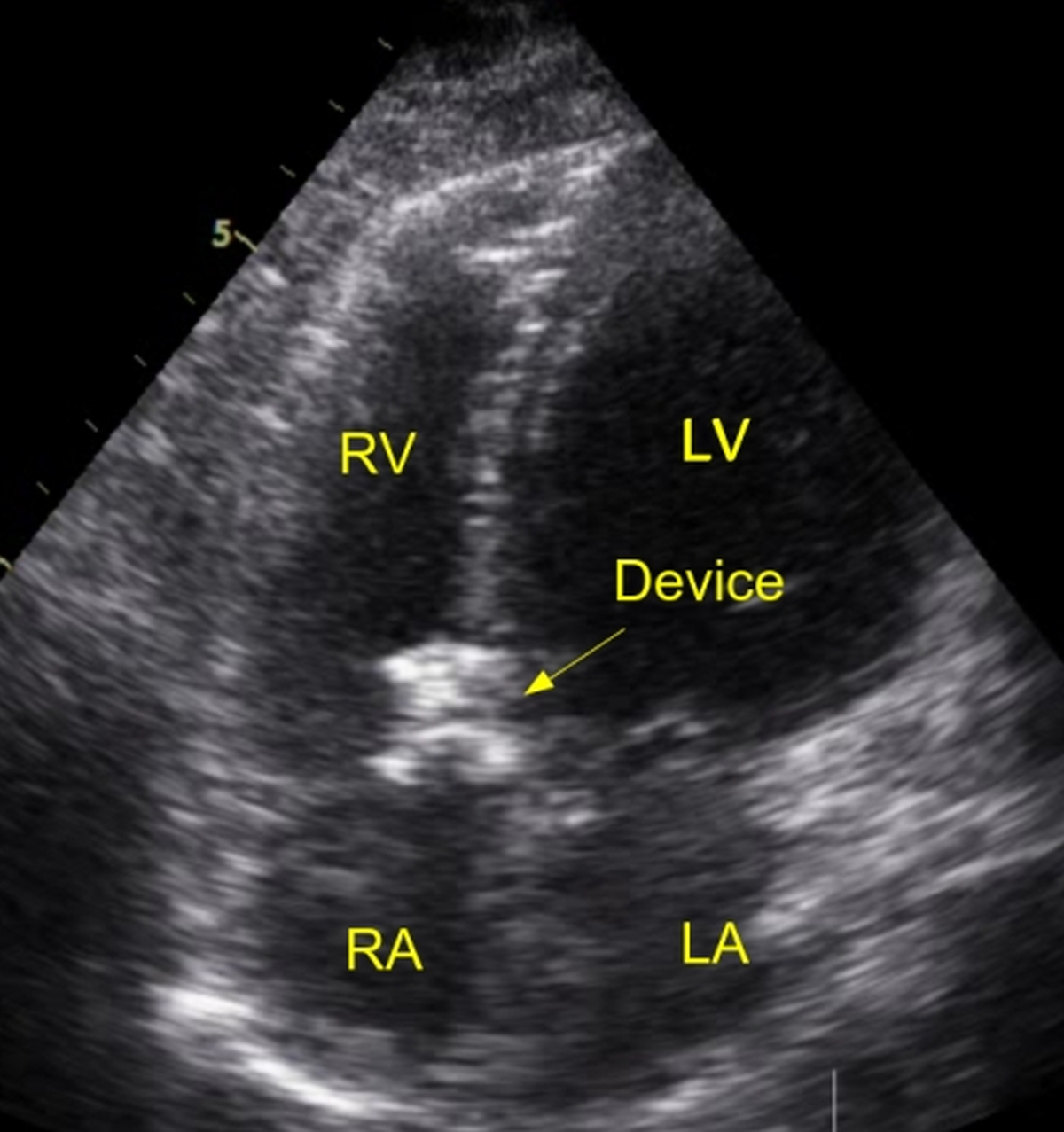
Device closure of RSOV is another option being increasingly used in suitable cases. The distance from the aortic end of the RSOV to the coronary ostium is specifically measured to check whether the device will impede coronary flow. In a report of 25 cases, different devices were used and devices were deployed using anterograde and retrograde approaches. A procedural success rate of 84% was achieved, including two patients who presented with cardiogenic shock. Two patients had residual leak and there was one case of device embolization. In one case, there was device induced severe aortic regurgitation. Associated ventricular septal defect was closed simultaneously in one patient. Three patients were referred for surgery. Overall, the authors preferred anterograde approach using duct occluders in most cases and muscular ventricular septal defect occluders in select cases [8].
References
- Moustafa S, Mookadam F, Cooper L, Adam G, Zehr K, Stulak J, Holmes D. Sinus of Valsalva aneurysms–47 years of a single center experience and systematic overview of published reports. Am J Cardiol. 2007 Apr 15;99(8):1159-64. doi: 10.1016/j.amjcard.2006.11.047. Epub 2007 Feb 28. PMID: 17437748.
- Yan F, Huo Q, Qiao J, Murat V, Ma SF. Surgery for sinus of valsalva aneurysm: 27-year experience with 100 patients. Asian Cardiovasc Thorac Ann. 2008 Oct;16(5):361-5. doi: 10.1177/021849230801600504. PMID: 18812342.
- Post MC, Braam RL, Groenemeijer BE, Nicastia D, Rensing BJ, Schepens MA. Rupture of right coronary sinus of Valsalva aneurysm into right ventricle. Neth Heart J. 2010 Apr;18(4):209-11. doi: 10.1007/BF03091763. PMID: 20428420; PMCID: PMC2856870.
- Weijerse A, van der Schoot MJ, Maat LP, Bruning TA, Geleijnse ML, Bogers AJ. Cardiac tamponade due to a ruptured aneurysm of the sinus of valsalva. J Card Surg. 2008 May-Jun;23(3):256-8. doi: 10.1111/j.1540-8191.2007.00520.x. PMID: 18435644.
- Hirapur I, Veeranna RM, Agrawal N. Classical windsock deformity of ruptured sinus of Valsalva: an unusual appearance on transthoracic echocardiography. BMJ Case Rep. 2014 May 26;2014:bcr2014204493. doi: 10.1136/bcr-2014-204493. PMID: 24862606; PMCID: PMC4039973.
- Lillehei Cw, Stanley P, Varco Rl. Surgical treatment of ruptured aneurysms of the sinus of Valsalva. Ann Surg. 1957;146:459–72
- Jung SH, Yun TJ, Im YM, Park JJ, Song H, Lee JW, Seo DM, Lee MS. Ruptured sinus of Valsalva aneurysm: transaortic repair may cause sinus of Valsalva distortion and aortic regurgitation. J Thorac Cardiovasc Surg. 2008 May;135(5):1153-8. doi: 10.1016/j.jtcvs.2008.01.004. PMID: 18455598.
- Mahimarangaiah J, Chandra S, Subramanian A, Srinivasa KH, Usha MK, Manjunath CN. Transcatheter closure of ruptured sinus of Valsalva: Different techniques and mid-term follow-up. Catheter Cardiovasc Interv. 2016 Feb 15;87(3):516-22. doi: 10.1002/ccd.26107. Epub 2015 Aug 10. PMID: 26255646.
