Surgery for tetralogy of Fallot
Surgery for tetralogy of Fallot
Tetralogy of Fallot is the commonest cyanotic congenital heart disease. Surgical repair has improved remarkably ever since it was first published in 1955 by Lillehei CW et al [1]. Excellent long term survival is now feasible, with 30 year survival ranging from 68.5% to 90.5% [2].
Symptomatic infants with tetralogy of Fallot can undergo either primary surgical repair or a palliative procedure which could be either a systemic to pulmonary shunt or catheter based right ventricular outflow tract or pulmonary valve dilatation [3]. A retrospective study using the UK National Congenital Heart Disease Audit had 1662 infants with mean age of 181 days from 2000 to 2013. Of these 1244 underwent primary surgical repair, 311 surgical systemic to pulmonary shunts and 107 right ventricular outflow tract dilatation procedures. Mortality was higher in those who underwent primary repair before 60 days of age. Mortality at 12 years was 18.7% in those repaired before the age of 60 days vs 2.2% for those repaired after that. Right ventricular outflow tract dilatations was associated with more right ventricular outflow tract reinterventions and fewer pulmonary valve replacements at 12 years. They had lower mortality after complete repair.
While considering procedures in early life, each has its own disadvantages. Early primary repair can increase the need for transannular patch and late morbidity, mostly due to pulmonary regurgitation. Surgical shunts have high rates of complications, while right ventricular outflow tract dilatation procedures are associated with valve lesions and reinterventions [3]. Surgical shunts in congenital heart disease have been detailed earlier.
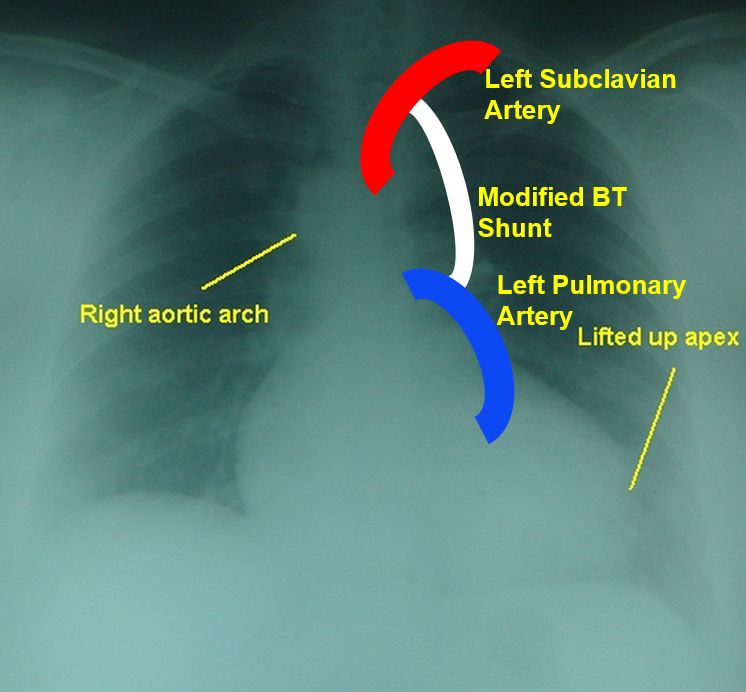
Schematic diagram of a modified Blalock-Taussig shunt in a person with right aortic arch and tetralogy of Fallot is illustrated here.
The initial surgical repair was by a ventriculotomy approach in the right ventricular anterior wall and transannular patch was used to relieve right ventricular outflow tract obstruction if needed. 26-31 year follow up of the first 106 patients was published in 1986. They mentioned that the first surgical correction was done on August 31, 1954 [4]. Initial 6 patients were operated by cross circulation and remaining 100 patients with bubble oxygenator. They noted that actuarial survival at 30 years was 77%. Actuarial freedom from reoperations at 30 years was 91%. An excellent aspect is that 32% completed college, 5 took masters degrees, 2 MDs, 2 PhDs and one lawyer! Forty patients had progeny with 93% live births and six major cardiac defects.
To avoid a ventriculotomy, transatrial and transatrial-transpulmonary approach is currently preferred for repair of tetralogy of Fallot. In a long term follow up data of 453 patients who underwent transatrial-transpulmonary repair at a median age of 0.6 years, survival was 97.3% at a median follow up of 14.3 years (range 0.1-42.1 years). Transannular patch was used in 65% of patients, though use declined over time from 89% initially to 64% later. Primary outcome measures in that retrospective analysis were death, pulmonary valve replacement, reintervention for other reasons and implantation of a cardioverter defibrillator or pacemaker. The use of a transannular patch was a predictor for poorer event free outcomes, with 1.7 times risk of composite endpoint [5]. 52 patients underwent pulmonary valve replacement and 5 had pacemaker insertion during follow up.
References
- Lillehei CW, Cohen M, Warden HE, Read RC, Aust JB, Dewall RA, Varco RL. Direct vision intracardiac surgical correction of the tetralogy of Fallot, pentalogy of Fallot, and pulmonary atresia defects; report of first ten cases. Ann Surg. 1955 Sep;142(3):418-42.
- van der Ven JPG, van den Bosch E, Bogers AJCC, Helbing WA. Current outcomes and treatment of tetralogy of Fallot. F1000Res. 2019 Aug 29;8:F1000 Faculty Rev-1530.
- Dorobantu DM, Mahani AS, Sharabiani MTA, Pandey R, Angelini GD, Parry AJ, Tulloh RMR, Martin RP, Stoica SC. Primary repair versus surgical and transcatheter palliation in infants with tetralogy of Fallot. Heart. 2018 Nov;104(22):1864-1870.
- Lillehei CW, Varco RL, Cohen M, Warden HE, Gott VL, DeWall RA, Patton C, Moller JH. The first open heart corrections of tetralogy of Fallot. A 26-31 year follow-up of 106 patients. Ann Surg. 1986 Oct;204(4):490-502.
- Luijten LW, van den Bosch E, Duppen N, Tanke R, Roos-Hesselink J, Nijveld A, van Dijk A, Bogers AJ, van Domburg R, Helbing WA. Long-term outcomes of transatrial-transpulmonary repair of tetralogy of Fallot. Eur J Cardiothorac Surg. 2015 Mar;47(3):527-34.
