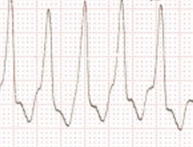
Wide QRS tachycardia
Wide QRS tachycardia
Wide QRS Tachycardia
Electrocardiographic recognition of ventricular tachycardia (VT) by the presence of:
-
- A V dissociation – P waves randomly distributed
-
- Capture beats and fusion beats
- Monomorphic with concordant QRS pattern in chest leads
Sustained vs Nonsustained VT:
Sustained > 30 sec
Non-sustained at least 6 beats, but less than 30 sec
Types of LVOT VT: supracuspal vs infracuspal
Mechanisms of VT:
-
- Re-entrant: Types of re-entrant circuits: Anatomic, functional, anisotropic
-
- Automatic
- Triggered activity – Early after depolarisation and Delayed after depolarisation
Identification of VT – Tips
Septal VT has a relatively narrower QRS
If the QRS complex in tachycardia is narrower than in sinus rhythm it favors ventricular tachycardia originating from ventricle with the blocked bundle branch.
Concordant QRS in chest leads – Negative concordance in apical origin; Positive concordance in basal origin
LBBB pattern – RV or LV septum
RBBB – LV origin; RBBB pattern with abrupt loss of R wave seen in VT following anteroapical infarction
Fascicular VT: RBBB pattern, relatively narrower QRS complex, verapamil sensitive.
Posterior fascicular: left axis deviation; anterior fascicular: right axis deviation; septal fascicular VT: normal axis
Idiopathic Ventricular Tachycardia:
Absence of structural heart disease
Symptoms not generally severe
More often in young adults
May be an important cause of tachycardia
Cardiac arrest is rare
VT from RVOT usually occurs in salvoes (Gallavardin). No associated structural heart disease.
It has an LBBB morphology with right axis, exercise induced, catecholamine sensitive and adenosine sensitive due to the mechanism of triggered activity. ARVC also gives rise to VT mimicking idiopathic RVOT VT.
VT in the absence of structural heart disease:
RVOT / LVOT ventricular tachycardias and ILVT (Idiopathic Left Ventricular Tachycardia)
Channelopathies – LQTS, Brugada
Therapy in Long QT syndrome:
Beta blockers – highly effective
Pacemakers
ICD: Rochester ICD-LQTS registry: Interim data presented at HRS 2008:
Females had a higher discharge rate, Those with QT more than 500ms and a history of syncope had higher discharge rate. LQT2 had the maximum chance of ICD discharge. Dual mutation also conferred higher chance of ICD discharge.
Pacemakers useful in pause dependent torsades or if bradycardia develops due to beta blockers.
Who should get an ICD in Brugada syndrome?
Baseline abnormal ECG (without drug challenge), male patient and symptomatic patient have a higher risk. Inducible tachycardia also carries a higher risk.