Jugular venous pulse (JVP)
Jugular venous pulse (JVP)
Assessment of jugular venous pulse has to be done in the internal jugular vein though a beginner is often tempted to use the external jugular vein. External jugular vein may be kinked and it may not reflect the true right atrial pressure. Jugular venous pressure is measured with reference to the sternal angle. The sternal angle is 5 cm above the mid right atrium in all positions. Normal internal jugular venous pulsations are not visible in the neck in the sitting position. Hence it is typically assessed with 45 degrees propped up position.
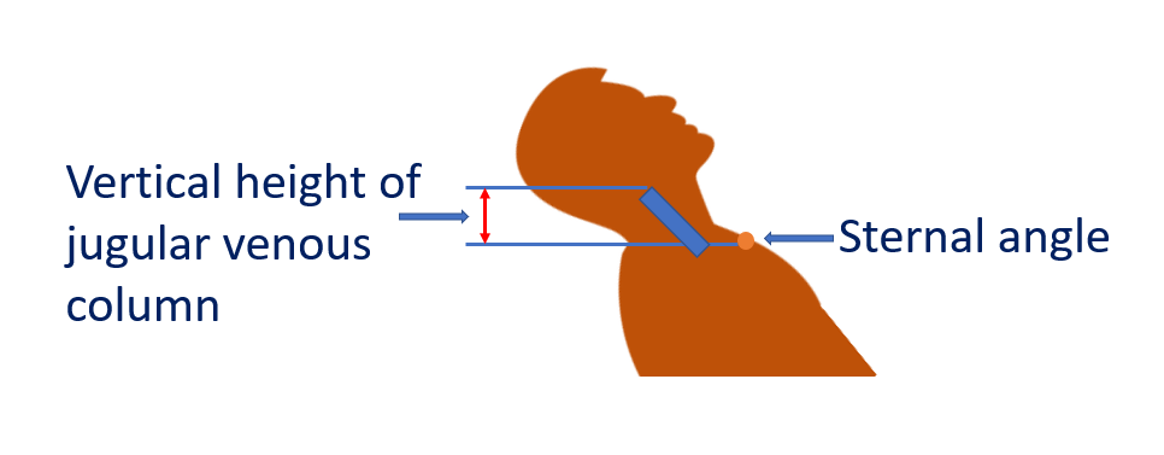
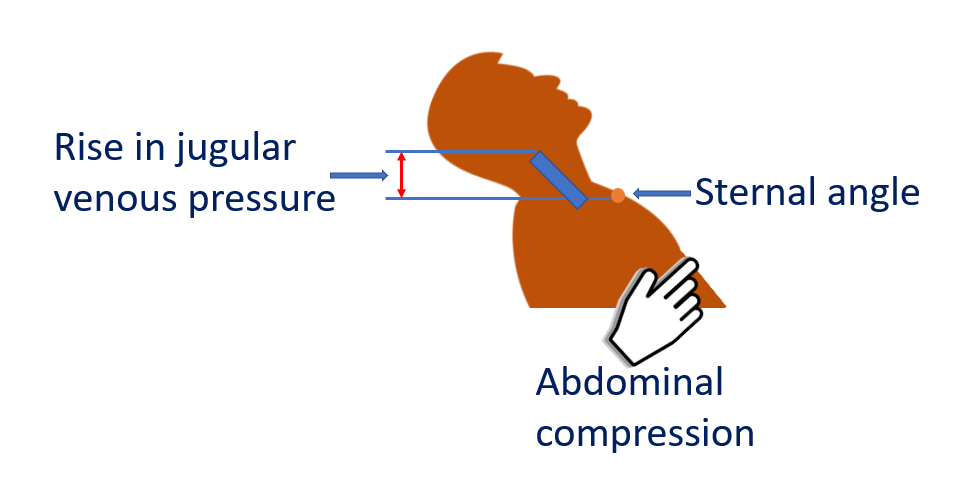
But if the venous pressure is elevated, evaluation in sitting position is possible. Vertical distance of the upper level of the pulsations above the sternal angle is checked and measured in cm of JVP. Sometimes the JVP may be so high that the upper level may not be visible. It may be visible in standing position in such cases. Pulsations of the ear lobe will be noted in such cases. In cases without visible elevation of JVP, sustained pressure over the upper abdomen for 30 seconds may be given to elicit the abdominojugular or hepatojugular reflux.
While examining engorged jugulars, it is important to check whether they are pulsatile or non-pulsatile. Non-pulsatile engorged jugulars suggest superior vena caval obstruction (Superior vena cava syndrome).
Respiratory variation of the jugular venous pulsation is another important aspect. Normally the amplitude of the pulsations increase in inspiration while the upper level (jugular venous pressure) falls in inspiration as the blood rushes into the right atrium. An inspiratory increase in jugular venous pressure is known as Kussmaul’s sign. It is seen in right heart failure and is a typical sign in constrictive pericarditis.
An often asked question is how to differentiate between venous and arterial pulsations in the neck. The usual answer is:
- Venous pulsations are better seen than felt.
- Venous pulsation has a definite upper level.
- Venous pulsation has multiple waves in a cardiac cycle while the arterial pulsation usually has only a single wave.
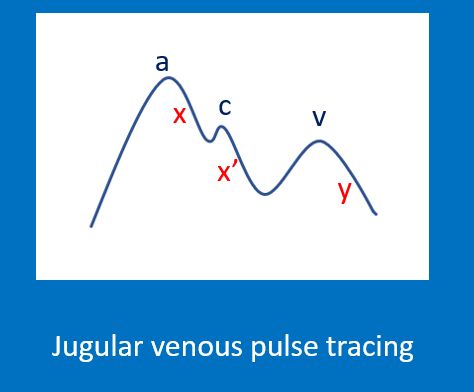
Jugular venous pulse tracing resembles right atrial pressure tracing.
- It has three positive waves: a, c and v
- It has two negative waves: x and y descents. An x’ (x prime) descent may be seen after the c wave.
During clinical examination, the descents are better appreciated than the waves, of which y descent is the most prominent. On visual inspection, only a and v waves are visible while c wave can be documented only in a pulse recording.
a wave is due to atrial contraction. It is prominent in tricuspid stenosis, pulmonary stenosis and pulmonary hypertension. Prominent a wave does not occur in an unrestricted ventricular septal defect. Intermittent large a waves may be seen in complete heart block when atrial contraction occurs with a closed tricuspid valve. These are called cannon waves. a wave is absent in atrial fibrillation as there is no organized atrial contraction.
c wave in jugular venous pulse is a carotid artifact while in the atrial pressure tracing it is due to bulging of the atrioventricular valve during ventricular contraction.
v wave occurs during venous filling after the ventricular contraction. In tricuspid regurgitation, c and waves fuse together to form a prominent cv wave. It is also called just a prominent v wave.
x descent is absent in tricuspid regurgitation.
Y descent can be prominent in constrictive pericarditis and is known as Friedreich’s sign. y descent is shallow in tricuspid stenosis. In cardiac tamponade, the y descent is absent.