Rheumatic aortic stenosis
Rheumatic aortic stenosis
Aortic stenosis in rheumatic heart disease seldom occurs alone, but in combination with aortic regurgitation or other valvular lesions. Isolated aortic stenosis is most commonly congenital in younger age group and degenerative in the elderly.
In severe aortic stenosis, the left ventricle hypertrophies as a compensatory mechanism. The type of hypertrophy is known as concentric left ventricular hypertrophy. In concentric hypertrophy, there is thickening of the left ventricular wall without enlargement of the left ventricular cavity. In late stages as the left ventricle fails, it may dilate.
Important symptoms of aortic stenosis are effort angina, exertional dyspnea and exertional syncope. Effort angina occurs due to the mismatch between coronary arterial blood supply and the demand of a hypertrophied left ventricle. Exertional syncope occurs due to fixed cardiac output. When there is peripheral vasodilation with exercise, the fixed cardiac output causes cerebral hypoperfusion and syncope.
Important physical findings of aortic stenosis include a slow rising low volume pulse (pulsus parvus et tardus), heaving apex (sustained and forceful), soft aortic component of second heart sound, ejection click and an ejection systolic murmur in aortic area. The murmur of aortic stenosis is conducted to the carotids and may associated with a thrill in aortic area. It may be necessary to feel in held expiration to feel a less prominent thrill. Ejection click of aortic stenosis is non-phasic, with no significant variation with respiration.
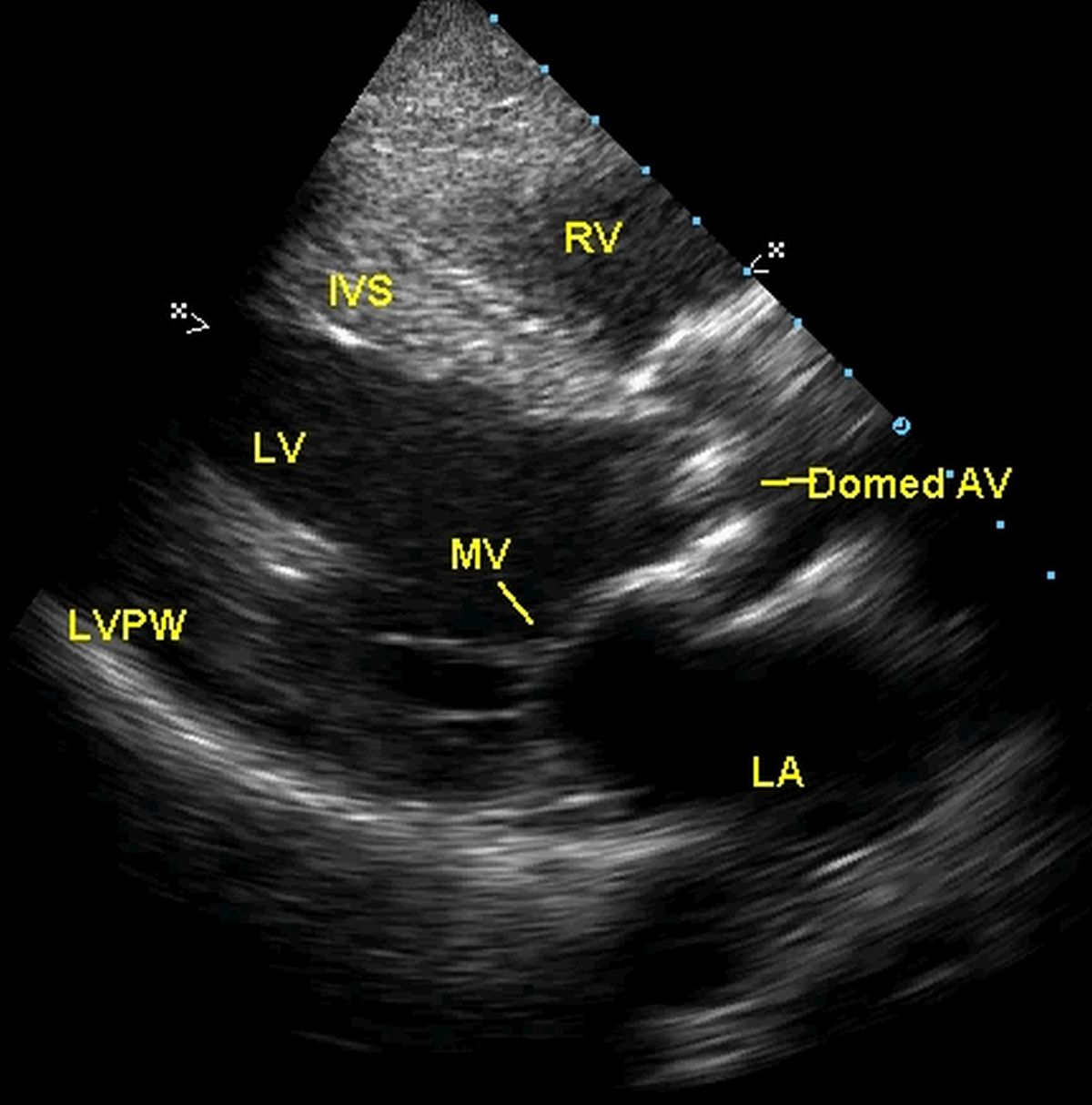
Echocardiogram from the left parasternal region showing thickened and doming aortic valve in severe aortic stenosis (Domed AV). RV: Right ventricle, IVS: Interventricular septum, LV: Left ventricle, MV: Mitral valve, LVPW: Left ventricular posterior wall, LA: Left atrium. Left ventricle is hypertrophied, as evidenced by the thickened interventricular septum.
Severe symptomatic aortic stenosis can be treated by aortic valve replacement either with a mechanical prosthesis or a bioprosthetic valve. Recently transcatheter aortic valve implantation (TAVI), also known as transcatheter aortic valve replacement (TAVR) has been introduced as a novel therapy. This approach is growing momentum, though a bit expensive currently. TAVI has been done mostly for the degenerative aortic stenosis of the elderly than rheumatic aortic stenosis.
Surgical repair of rheumatic aortic stenosis is another option in view of the long term problems of a prosthetic valve in young persons [1]. Various procedures described are decortication or peeling of the rheumatic thickening, shaving off and thinning the valve, commissurotomy and decalcification. Repair may be considered for mild to moderate aortic lesions during concomitant mitral valve surgery with acceptable results. Repair can also be considered in young persons where the cumulative long term problems of a prosthetic valve is more.
Any procedure has to be done before the left ventricle starts dilating due to irreversible fibrotic changes in the left ventricular myocardium. But since aortic stenosis is an afterload mismatch condition, the chance for improvement is more than in aortic regurgitation of corresponding severity and left ventricular dysfunction. In aortic stenosis, the left ventricle has a chance of recovering once the afterload mismatch is removed.
A report of 30 patients with rheumatic aortic stenosis in patients <30 years presenting with associated mitral stenosis has been published [2]. Three of the patients had additional tricuspid stenosis. History of rheumatic polyarthritis was given by 28 patients. Interestingly, the murmur of aortic stenosis was absent initially in 8 out of 10 patients who presented in congestive heart failure. All the patients underwent cardiac catheterization. Cineangiography showed trileaflet aortic valve, unlike in congenital aortic stenosis. Raised pulmonary vascular resistance was found in 87% patients.
References
- Afifi A, Hosny H, Yacoub M. Rheumatic aortic valve disease-when and who to repair? Ann Cardiothorac Surg. 2019 May;8(3):383-389.
- Vijayaraghavan G, Cherian G, Krishnaswami S, SUKUMAR IP, John S. Rheumatic aortic stenosis in young patients presenting with combined aortic and mitral stenosis. Br Heart J. 1977 Mar;39(3):294-8.