Ventricular septal defect
Ventricular septal defect
Ventricular septal defects (VSD) can be divided into perimembranous, muscular, inlet and outlet VSDs, depending on the location. Of these perimembranous VSDs are the commonest. VSDs can decrease in size and undergo spontaneous closure. Spontaneous closure is most likely with small muscular and perimembranous VSD, while inlet and outlet VSDs are least likely to close.
Perimembranous ventricular septal defect
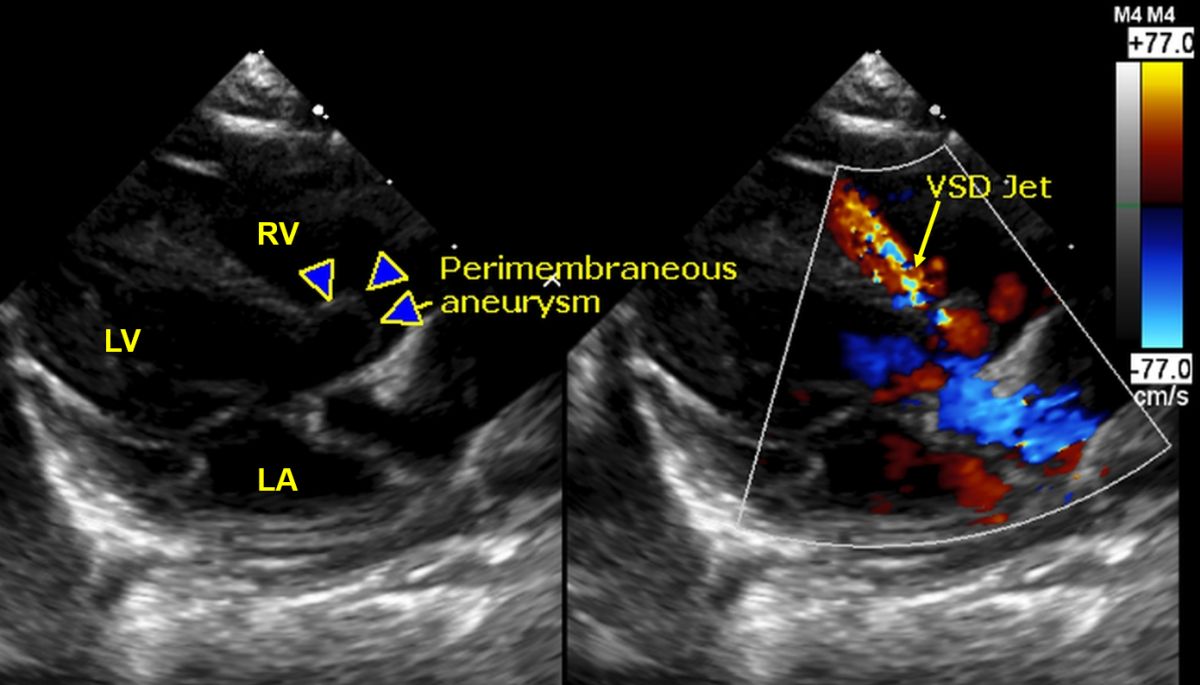
Echocardiogram in ventricular septal defect: Parasternal long axis view shows the subaortic perimembranous ventricular septal aneurysm (marked by arrows). The color mosaic jet from the left ventricular outflow tract into the right ventricle is seen in the right panel (VSD Jet). There is a perimembranous aneurysm meaning the VSD is on the closure path.
Perimembranous VSD is located in the left ventricular outflow tract and if large can involve the muscular septum in addition to the perimembranous septum. The mechanisms of spontaneous closure include:
1. Closure by aneurysm formation
2. Closure by prolapse of the aortic valve
3. Closure by attachment of septal tricuspid leaflet
4. Closure by ingrowth of tissue
When prolapse of aortic valve occurs, there is associated aortic regurgitation which can progress over the years. Similarly, when the closure is by attachment of the septal tricuspid leaflet, there can be tricuspid regurgitation. If there is a fenestration of the tricuspid leaflet, there is a left ventricle to right atrium shunt (LV-RA shunt). The other cause of LV-RA shunt is an atrioventricular septal defect or Gerbode VSD.
Muscular ventricular septal defect
Muscular VSD can be anywhere along the muscular septum and can be multiple. Multiple muscular VSDs are known as Swiss cheese VSD and are difficult to close surgically. Small apical muscular VSD has a soft apical systolic murmur of shorter duration unlike the loud pan systolic murmur in the parasternal region of the other VSDs. This is because the defect is occluded by ventricular muscle contraction in the latter part of the systole.
Inlet ventricular septal defect
Inlet ventricular septal defect is part of the endocardial cushion defects and can be associated with ostium primum atrial septal defect and atrioventricular valve regurgitation. The ventricular septal defect associated with Down syndrome is usually of this type. If both inlet VSD and ostium primum atrial septal defect are present, then it is called a complete atrioventricular (AV) canal defect. Other name for inlet VSD is canal VSD. A cleft in the mitral valve is the reason for the associated mitral regurgitation. Atrioventricular conduction abnormalities may be associated. When there is a complete AV canal defect, a common atrioventricular valve can be present.
Outlet ventricular septal defect
Outlet VSDs are also called subpulmonic VSD and doubly committed VSD and subarterial VSD as they are located in the right ventricular outflow tract in relation to both the great vessels. These VSDs are more common in the far East and more likely to have associated aortic regurgitation. Chance for spontaneous closure is low in these and some advocate surgical closure even for outlet VSD to prevent future development of progressive aortic regurgitation.
Clinical findings in VSD
Clinical findings depend on size and location of the defect. A small defect produces a loud murmur (maladie de Roger), often associated with a thrill in the parasternal region, while the murmur is soft or even inaudible in a large VSD. This is because the pressure in the two ventricles equalizes in large VSD. The murmur may disappear when severe pulmonary hypertension develops and the left to right shunt ceases and a right to left shunt ensues (Eisenmenger reaction). Severe pulmonary hypertension develops when there is a large left to right shunt from early infancy due to pulmonary vasoreactivity. In late stages, obliterative changes may occur in the pulmonary vasculature. When this occurs, it is irreversible even after surgical or device closure of the VSD. When there is pulmonary hypertension, there is a loud pulmonary component of second heart sound (P2) which may be palpable and associated with dullness on percussion in 2nd left intercostal space. Right ventricular hypertrophy in this situation is manifest as left parasternal heave. Cyanosis and clubbing occurs in Eisenmenger syndrome. Eisenmenger complex is the specific name for VSD Eisenmenger.
The VSD murmur may be higher up in outlet VSD and towards the apex in small apical muscular VSD. In inlet VSD, murmur of associated mitral regurgitation may be audible, but may be difficult to differentiate from VSD murmur.
Related Posts
-
Cardiac murmurs
No Comments | Sep 24, 2020
-
Congenital heart disease overview
No Comments | Oct 10, 2020
-
Chest X-ray – overview
No Comments | Sep 28, 2020
-
Coronary artery disease – overview and risk factors
No Comments | Oct 5, 2020
About The Author
Johnson Francis
Former Professor of Cardiology, Calicut Govt. Medical Kozhikode, Kerala, India. Editor-in-Chief, BMH Medical Journal